|   |
|   |
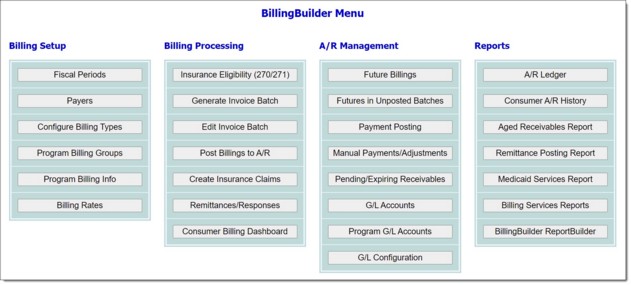
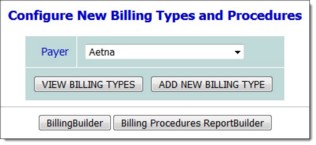
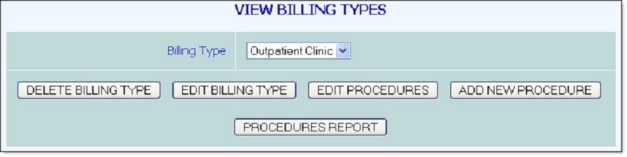
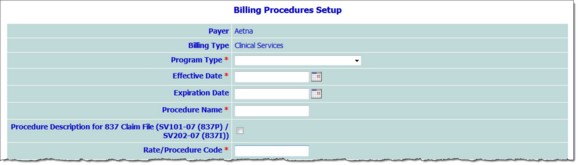
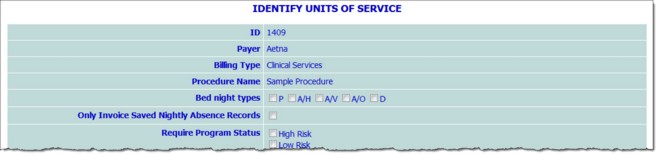
Procedure configuration follows billing type configuration in the setup process. In this step, each billing type must have one or more procedures created for it. For example, a "clinic" billing type may have a procedure called "individual counseling" set up for it.
Each procedure you create during this step will have documentation requirements that must be met in order to generate invoices. As a result, part of the procedure configuration process includes entering information about how services must be documented in AWARDS. For instance, for the "individual counseling" example there might be a requirement of a minimum number of minutes of face to face contact with a client in order for the procedure to be billable.
To configure a new procedure and set up its requirements, complete the following steps:
![]() TIP: The following instructions assume that you are beginning the procedure configuration process from the AWARDS Home screen; however, they may also be configured immediately after the associated billing type is entered/updated by clicking CONTINUE AND ADD PROCEDURES from the billing type confirmation page. When proceeding from there, skip ahead to step 8 below.
TIP: The following instructions assume that you are beginning the procedure configuration process from the AWARDS Home screen; however, they may also be configured immediately after the associated billing type is entered/updated by clicking CONTINUE AND ADD PROCEDURES from the billing type confirmation page. When proceeding from there, skip ahead to step 8 below.
![]() TIP: All programs in AWARDS belong to a particular program type. If you are not familiar with program types, please contact your Foothold Customer Success & Advocacy representative for guidance.
TIP: All programs in AWARDS belong to a particular program type. If you are not familiar with program types, please contact your Foothold Customer Success & Advocacy representative for guidance.
![]() NOTE: The program type selected here will determine which charting events, service types, progress note types, visit types, program statuses, and group activity types are available on the next page.
NOTE: The program type selected here will determine which charting events, service types, progress note types, visit types, program statuses, and group activity types are available on the next page.
![]() Effective Date - In this field, type the effective date for this procedure.
Effective Date - In this field, type the effective date for this procedure.
![]() TIP: AWARDS will only bill for services that occur after the Effective Date entered here.
TIP: AWARDS will only bill for services that occur after the Effective Date entered here.
![]() Expiration Date - In this field, type the expiration date for this procedure.
Expiration Date - In this field, type the expiration date for this procedure.
![]() TIP: Entering an Expiration Date will discontinue the procedure, making it un-billable once the expiration date occurs. This is generally utilized when a procedure is no longer billable, but needs to be saved in case the agency wants to back-bill for it.
TIP: Entering an Expiration Date will discontinue the procedure, making it un-billable once the expiration date occurs. This is generally utilized when a procedure is no longer billable, but needs to be saved in case the agency wants to back-bill for it.
![]() Procedure Name - In this field, type the procedure name.
Procedure Name - In this field, type the procedure name.
![]() Procedure Description for 837 Claim File (SV101-07 (837P) / SV202-07 (837I)) - In this field, type a description for the procedure to be reported in the 837 claim file.
Procedure Description for 837 Claim File (SV101-07 (837P) / SV202-07 (837I)) - In this field, type a description for the procedure to be reported in the 837 claim file.
![]() Rate/Procedure Code - In this field, type the procedure code.
Rate/Procedure Code - In this field, type the procedure code.
![]() TIP: This may also be referred to as the "rate code" or "CPT code."
TIP: This may also be referred to as the "rate code" or "CPT code."
![]() CPT/HCPCS & Modifier Code(s) - In this field, type the payer's CPT/HCPCS and modifier code(s) that need to be sent in the claim file/format when this procedure is invoiced, as detailed here:
CPT/HCPCS & Modifier Code(s) - In this field, type the payer's CPT/HCPCS and modifier code(s) that need to be sent in the claim file/format when this procedure is invoiced, as detailed here:
837I - SV202-2 and SV202-3 (loop 2400)
837P - SV101-2 and SV101-3 (loop 2400)
HCFA-1500 - Box 24D (CPT/HCPCS column and Modifier column)
UB-04 - Box 44
![]() TIP: Up to four modifier codes can be entered in addition to the five character CPT/HCPCS code. The code and any modifiers should each be separated with a colon (:) and no spaces as shown here:
TIP: Up to four modifier codes can be entered in addition to the five character CPT/HCPCS code. The code and any modifiers should each be separated with a colon (:) and no spaces as shown here:
One modifier: 12345:99
Two modifiers: 12345:99:88
Three modifiers: 12345:99:88:77
Four modifiers: 12345:99:88:77:66
|
For Monthly billing types: |
For Per Diem/Daily billing types: |
For Fee for Service billing types: |
|
Reception Desk - Attendance / Group Activities - Days Reception Desk - Attendance / Group Activities - Time Program Attendance - Admitted to Program Services - Progress Notes/Contacts Logs/Group Notes - Time Services - Progress Notes/Contacts Logs/Group Notes - Days Housing - Nightly Absences Operations - Transportation |
Services - Progress Notes/Contacts Logs/Group Notes Reception Desk - Attendance / Group Activities Housing - Nightly Absences Services - Transportation Operations - Transportation |
Services - Progress Notes/Contacts Logs/Group Notes Reception Desk - Attendance / Group Activities Housing - Nightly Absences Operations - Transportation |
![]() Equivalent Code - In this field, type an equivalent CPT/HCPCS code (no modifiers) if your agency has COB/waterfall billing and not all payers assigned to a client within their Entitlement records bill using the same code for the same service.
Equivalent Code - In this field, type an equivalent CPT/HCPCS code (no modifiers) if your agency has COB/waterfall billing and not all payers assigned to a client within their Entitlement records bill using the same code for the same service.
![]() TIP: Typically the CPT/HCPCS code for the secondary payer is entered in the Equivalent Code for the secondary payer's procedure, as well as the Equivalent Code for the primary payer's procedure, thus creating a related pair. For example:
TIP: Typically the CPT/HCPCS code for the secondary payer is entered in the Equivalent Code for the secondary payer's procedure, as well as the Equivalent Code for the primary payer's procedure, thus creating a related pair. For example:
Primary Payer's Procedure
CPT/HCPCS Code = 12345
Equivalent Code = 67890
Secondary Payer's Procedure
CPT/HCPCS Code = 67890
Equivalent Code = 67890
![]() Revenue Code - In this field, type the 837I revenue code associated with the CPT/HCPCS code. If a revenue code is not entered here, the revenue code for invoices associated with this procedure will be pulled from the Program Billing Info > Revenue Code field.
Revenue Code - In this field, type the 837I revenue code associated with the CPT/HCPCS code. If a revenue code is not entered here, the revenue code for invoices associated with this procedure will be pulled from the Program Billing Info > Revenue Code field.
![]() Locator Code - In this field, enter the default locator code for the procedure. If data is entered here, is will be used in place of the value entered in the Locator Code field from the Program Billing Info page.
Locator Code - In this field, enter the default locator code for the procedure. If data is entered here, is will be used in place of the value entered in the Locator Code field from the Program Billing Info page.
![]() NOTE: This option is only available if the procedure is associated with a billing type where the setting Whether to generate the 837I, 837P is set to "837I."
NOTE: This option is only available if the procedure is associated with a billing type where the setting Whether to generate the 837I, 837P is set to "837I."
![]() Incident To NPI - In this field, type the NPI, first name, and last name of the incident to provider that needs to be associated with the invoices for the procedure identified.
Incident To NPI - In this field, type the NPI, first name, and last name of the incident to provider that needs to be associated with the invoices for the procedure identified.
![]() IMPORTANT! Please note that this is a "hard override," meaning any data captured here will be placed on the invoice instead of the note writer's information (from Human Resources > Staff Information > Credentials > National Provider Identifier) or any default medical provider information (from Program Billing Info).
IMPORTANT! Please note that this is a "hard override," meaning any data captured here will be placed on the invoice instead of the note writer's information (from Human Resources > Staff Information > Credentials > National Provider Identifier) or any default medical provider information (from Program Billing Info).
![]() Incident To Taxonomy Code - In this field, type the taxonomy code associated with the incident to NPI. If data is entered in this field it will be present in the 837 claim if the "Incident to NPI" option above is filled in, and the "Send Rendering/Attending Provider Taxonomy Code in 837" option is checked off under Configure Payers.
Incident To Taxonomy Code - In this field, type the taxonomy code associated with the incident to NPI. If data is entered in this field it will be present in the 837 claim if the "Incident to NPI" option above is filled in, and the "Send Rendering/Attending Provider Taxonomy Code in 837" option is checked off under Configure Payers.
![]() Incident to Secondary ID - In this field enter the secondary ID associated with the Incident to NPI. In the corresponding 837 ID Qualifier field, enter the associated 837 ID qualifier ID. This data is reported in the "REF" 837 segment within the 2310B loop (837P) and the 2310A loop (837I).
Incident to Secondary ID - In this field enter the secondary ID associated with the Incident to NPI. In the corresponding 837 ID Qualifier field, enter the associated 837 ID qualifier ID. This data is reported in the "REF" 837 segment within the 2310B loop (837P) and the 2310A loop (837I).
![]() Service Facility Info for 837 - If the procedures associated payer has the Report Service Facility Info in 837 option checked, click the radio button here that indicates where the 837 service facility information should be reported from for the procedure. Available options are:
Service Facility Info for 837 - If the procedures associated payer has the Report Service Facility Info in 837 option checked, click the radio button here that indicates where the 837 service facility information should be reported from for the procedure. Available options are:
Use Program Billing Info - When selected, all service facility information for the procedure will be reported from "Service Facility Information" section of the Program Billing Info page.
Use Procedure Override Options - When selected, all service facility information for the procedure will be reported from input fields under the Use Procedure Override Options option on the procedure configuration screen. (The input fields are only displayed if the corresponding option radio button is selected.)
Use Staff HR Info - When selected, all service facility information for the procedure will be reported from the note writer's staff information record (Human Resources > Staff Information > Demographics tab > Street Address and City, State, Zip fields - AND - Credentials tab > National Provider Identifier and Rendering/Attending Provider Secondary ID, 837 Qualifier fields). If multiple notes are used to generate an invoice for the procedure, AWARDS will use the note writer information associated with the first progress note written for the consumer/day (oldest progress note ID).
Use Billing Info Tab in Agency Program Information - When selected, all service facility information for the procedure will be reported form the Billing Info Tab under System Setup > Agency Program Info > Add/Edit Entire Program. On that tab distinct service facility information can be entered for each note location by selecting the locations radio button and filling in the corresponding fields. If multiple notes are used to generate an invoice for the procedure, AWARDS will use the note location information associated with the first progress note written for the consumer/day (oldest progress note ID).
![]() Authorization is required - Click this checkbox if the payer requires prior authorization for this procedure.
Authorization is required - Click this checkbox if the payer requires prior authorization for this procedure.
![]() TIP: If authorization is required, a client's authorization information is entered in the "BillingBuilder Insurance Authorizations" section of the Certified Entitlements feature, accessible from within the Entitlements module or from the client's face sheet.
TIP: If authorization is required, a client's authorization information is entered in the "BillingBuilder Insurance Authorizations" section of the Certified Entitlements feature, accessible from within the Entitlements module or from the client's face sheet.
![]() TIP: If a billing procedure is configured to require authorization, then AWARDS will not bill for a client for that procedure unless there is a current authorization record found in that client's entitlements.
TIP: If a billing procedure is configured to require authorization, then AWARDS will not bill for a client for that procedure unless there is a current authorization record found in that client's entitlements.
![]() Do not send Authorization Number in claims - Click this checkbox if the authorization number is NOT to be sent in the claim file. AWARDS will continue to decrement/count down the total remaining service/units as billable services are rendered.
Do not send Authorization Number in claims - Click this checkbox if the authorization number is NOT to be sent in the claim file. AWARDS will continue to decrement/count down the total remaining service/units as billable services are rendered.
![]() Valid Diagnosis DSM/ICD Heading - In this field, type a comma-delimited list of the ICD diagnoses required for the billing procedure. For example, if you are allowed to bill ICD codes that begin with F, S, and Q, then enter F,S,Q here. If you are allowed to bill only ICD codes that begin with F3, enter F3 here.
Valid Diagnosis DSM/ICD Heading - In this field, type a comma-delimited list of the ICD diagnoses required for the billing procedure. For example, if you are allowed to bill ICD codes that begin with F, S, and Q, then enter F,S,Q here. If you are allowed to bill only ICD codes that begin with F3, enter F3 here.
![]() TIP: If a value is entered here it will override the data entered at the billing type level. Only enter data here if the settings on the Billing Type page do not apply to the procedure.
TIP: If a value is entered here it will override the data entered at the billing type level. Only enter data here if the settings on the Billing Type page do not apply to the procedure.
![]() Additional eligibility entitlement is required - This drop-down list is populated with those insurances/eligibilities available for selection under Entitlements. If appropriate, use this option to select a second eligibility required in order to bill for this procedure.
Additional eligibility entitlement is required - This drop-down list is populated with those insurances/eligibilities available for selection under Entitlements. If appropriate, use this option to select a second eligibility required in order to bill for this procedure.
![]() Rendering/Attending Provider in 837 - Click one of the following radio buttons to indicate where the rendering/attending provider data should be reported in the 837 file, or if this data should be omitted.
Rendering/Attending Provider in 837 - Click one of the following radio buttons to indicate where the rendering/attending provider data should be reported in the 837 file, or if this data should be omitted.
Report Rendering/Attending Provider in Claim Loop (2310B)
Report Rendering Provider in Service Loop (2420A)
Omit Rendering/Attending Provider Data
![]() Referring Provider is Required in 837 - Click this checkbox to have the referring provider name and NPI sent in the 837 electronic billing files alongside a rendering provider or in its place. Select a provider role from the corresponding drop-down list to have the name and NPI contained within the support services contacts section of a client's face sheet associated with the provider role you selected sent as the referring provider.
Referring Provider is Required in 837 - Click this checkbox to have the referring provider name and NPI sent in the 837 electronic billing files alongside a rendering provider or in its place. Select a provider role from the corresponding drop-down list to have the name and NPI contained within the support services contacts section of a client's face sheet associated with the provider role you selected sent as the referring provider.
![]() TIP: Checking the Not required, send data if present option will send referring provider information in the 837 claim file it if exists within the Support Services Contacts section of a client's face sheet and is associated with the provider role you chose to be sent as the referring provider.
TIP: Checking the Not required, send data if present option will send referring provider information in the 837 claim file it if exists within the Support Services Contacts section of a client's face sheet and is associated with the provider role you chose to be sent as the referring provider.
And report a Secondary ID - Click this checkbox to also report a referring provider secondary ID and the 837 claim file alongside a referring provider NPI. Once this box is checked, the referring provider secondary ID qualifier also needs to be entered in the 837 ID Qualifier field.
![]() NOTE: In the 837 Institutional electronic billing file this is loop 2310F, segment NM1 and in the 837 Professional electronic billing file this is loop 2310A, segment NM1.
NOTE: In the 837 Institutional electronic billing file this is loop 2310F, segment NM1 and in the 837 Professional electronic billing file this is loop 2310A, segment NM1.
![]() NOTE: If a referring provider secondary ID is reported, the data will appear in REF segment within the same loops as the NPI for both the 837I and 837P electronic billing files.
NOTE: If a referring provider secondary ID is reported, the data will appear in REF segment within the same loops as the NPI for both the 837I and 837P electronic billing files.
![]() Require Ordering Provider in 837P - Click this checkbox to have the ordering provider name and NPI sent in the 837 electronic billing files. From the corresponding drop-down list, select a provider role. The name and NPI of the individual in this role for the client (as recorded in the client's support services contacts on the face sheet) is sent as the ordering provider.
Require Ordering Provider in 837P - Click this checkbox to have the ordering provider name and NPI sent in the 837 electronic billing files. From the corresponding drop-down list, select a provider role. The name and NPI of the individual in this role for the client (as recorded in the client's support services contacts on the face sheet) is sent as the ordering provider.
![]() TIP: Checking the Not required, send data if present option will send ordering provider information in the 837 claim file if it exists within the Support Services Contacts portion of a client's face sheet and is associated with the provider role you chose to be sent as the ordering provider.
TIP: Checking the Not required, send data if present option will send ordering provider information in the 837 claim file if it exists within the Support Services Contacts portion of a client's face sheet and is associated with the provider role you chose to be sent as the ordering provider.
![]() NOTE: In the 837 Professional electronic billing file this is look 2420E, segment NM1*DK.
NOTE: In the 837 Professional electronic billing file this is look 2420E, segment NM1*DK.
![]() Referring Provider is Required in HCFA-1500 - Click this checkbox to have the referring provider name and NPI sent in the HCFA 1500 claim form in box 17 and 17b. Select a provider role from the corresponding drop-down list to have the name and the NPI contained within the Support Services Contacts section of a client's face sheet associated with the provider role you selected sent as the referring provider.
Referring Provider is Required in HCFA-1500 - Click this checkbox to have the referring provider name and NPI sent in the HCFA 1500 claim form in box 17 and 17b. Select a provider role from the corresponding drop-down list to have the name and the NPI contained within the Support Services Contacts section of a client's face sheet associated with the provider role you selected sent as the referring provider.
![]() TIP: Checking the Not required, send data if present option will send referring provider information in the HCFA-1500 claim file if it exists within the Support Services Contacts section of a client's face sheet and is associated with the provider role you chose to be sent as the referring provider.
TIP: Checking the Not required, send data if present option will send referring provider information in the HCFA-1500 claim file if it exists within the Support Services Contacts section of a client's face sheet and is associated with the provider role you chose to be sent as the referring provider.
And report a Secondary ID - Click this checkbox to also report a referring provider secondary ID in the HCFA-1500 paper claim form alongside a referring provider NPI. Once this option is checked, the referring provider secondary ID qualifier also needs to be entered in the HCFA-1500 ID Qualifier field.
![]() NOTE: If a referring provider secondary ID is reported, the data will appear in box 17a of the HCFA-1500 paper claim form as follows: HCFA-1500 Qualifier (small shaded box) and referring provider secondary ID (large shaded box).
NOTE: If a referring provider secondary ID is reported, the data will appear in box 17a of the HCFA-1500 paper claim form as follows: HCFA-1500 Qualifier (small shaded box) and referring provider secondary ID (large shaded box).
![]() Require Supervising Provider in 837P - Click this checkbox to require and have the supervising provider selected within a progress note or group note sent in the 837P electronic billing files.
Require Supervising Provider in 837P - Click this checkbox to require and have the supervising provider selected within a progress note or group note sent in the 837P electronic billing files.
And report a Secondary ID - Click this checkbox to also report a supervising provider secondary ID in the 837 claim file alongside a supervising provider NPI. Once this option is checked, the supervising provider secondary ID qualifier also needs to be entered in the 837 ID Qualifier field.
![]() IMPORTANT! For this option to work correctly, the Supervising Provider drop-down option must be turned on for both progress notes and group notes. To have this option added for both note types, please contact the Help Desk for assistance.
IMPORTANT! For this option to work correctly, the Supervising Provider drop-down option must be turned on for both progress notes and group notes. To have this option added for both note types, please contact the Help Desk for assistance.
![]() NOTE: In the 837 Professional electronic billing file this is in loop 2310D, segment NM1*DQ. The supervising provider secondary ID is also reported in loop 2310D, but in the REF segment just below NM1*DQ.
NOTE: In the 837 Professional electronic billing file this is in loop 2310D, segment NM1*DQ. The supervising provider secondary ID is also reported in loop 2310D, but in the REF segment just below NM1*DQ.
![]() Send Covered Days/Length of Stay Data in 837I/UB-04 - Click this checkbox to report this information within the 837I file, as well as on the paper UB-04 claim form.
Send Covered Days/Length of Stay Data in 837I/UB-04 - Click this checkbox to report this information within the 837I file, as well as on the paper UB-04 claim form.
![]() NOTE: 837I - This data is reported within the segment labeled "HI*BE" and the value code used is "80"
NOTE: 837I - This data is reported within the segment labeled "HI*BE" and the value code used is "80"
UB-04 - This data is reported in either box 39, 40, or 41, and the value code used is "80"
![]() Claim Frequency Type Code - Click one of the following radio buttons to report the appropriate frequency type code. This code is assigned to invoices as they are posted to A/R within the Post Billings to A/R screen in BillingBuilder.
Claim Frequency Type Code - Click one of the following radio buttons to report the appropriate frequency type code. This code is assigned to invoices as they are posted to A/R within the Post Billings to A/R screen in BillingBuilder.
![]() NOTE: This option is only available if ALL of the following are true:
NOTE: This option is only available if ALL of the following are true:
![]() Foothold Technology has activated this option in your AWARDS database.
Foothold Technology has activated this option in your AWARDS database.
![]() Billing Type > Whether to generate the 837I, 837P has "837I" selected.
Billing Type > Whether to generate the 837I, 837P has "837I" selected.
![]() Billing Type > Billing Unit Type is set to "Daily/Per Diem."
Billing Type > Billing Unit Type is set to "Daily/Per Diem."
Report "1" Admit to Discharge Claim - The default setting. Select this option to always report a "1" on all invoices (other than manual adjustment or void invoices).
Assign Claim Frequency Type Code for Initial (2), Interim (3), and Discharge (4) invoices - Select this option to report 2, 3, or 4 based on which episode of care invoices is being invoiced for this consumer. (The first invoice for a consumer's program stay/procedure code will be assigned code 2. All other invoices will be assigned code 3. The last invoice will be assigned code 4 if the consumer's program discharge date is within the timeframe of the batch being generated.)
Override Fourth Character in Box 4 of UB-04 - Click this option and enter a value in the corresponding text box to always report a specific fourth character in box 4 of the paper UB-04 claim form.
![]() Generate One Invoice from Consumers Program Admission to Discharge - Click this checkbox to generate one invoice for a consumer based on his/her entire program stay for the procedure. The invoice will be generated if the batch date range contains the consumer's discharge date.
Generate One Invoice from Consumers Program Admission to Discharge - Click this checkbox to generate one invoice for a consumer based on his/her entire program stay for the procedure. The invoice will be generated if the batch date range contains the consumer's discharge date.
![]() NOTE: This procedure option will only show if ALL of the following are true:
NOTE: This procedure option will only show if ALL of the following are true:
![]() The procedure is associated with a Daily/Per Diem billing type set to create the 837I file.
The procedure is associated with a Daily/Per Diem billing type set to create the 837I file.
![]() The Billable Documentation Type is "Housing - Nightly Absences"
The Billable Documentation Type is "Housing - Nightly Absences"
![]() TIP: The consumer's discharge date is not a billable date.
TIP: The consumer's discharge date is not a billable date.
![]() Omit Date Last Seen from Claims - Click this checkbox to omit the 837 segment "Last Seen Date (DPT*304)" from the 837P file.
Omit Date Last Seen from Claims - Click this checkbox to omit the 837 segment "Last Seen Date (DPT*304)" from the 837P file.
![]() Report NTE (Line Note) Segment in 837 - Click this checkbox to report the NTE segment in the 837P file. Once checked, enter the associated NTE reference code within the Note Reference Code text box. Lastly, click one of the following corresponding radio buttons:
Report NTE (Line Note) Segment in 837 - Click this checkbox to report the NTE segment in the 837P file. Once checked, enter the associated NTE reference code within the Note Reference Code text box. Lastly, click one of the following corresponding radio buttons:
Report Service Time - Select this option to report the start time and end time of the progress note or group note that created the invoice. This data will be reported as SVCSTIME(+2 blank spaces)note start and end time in military format; for example, SVCSTIME 1100-1200.
Report General Message - Select this option to report a general message each time the procedure is invoiced.
![]() NOTE: Please note the following regarding this procedure option:
NOTE: Please note the following regarding this procedure option:
![]() It is only available if the billable document type of "Services - Progress Notes/Contacts Logs/Group Notes" is selected and the procedure is associated with a Daily/Per Diem billing type.
It is only available if the billable document type of "Services - Progress Notes/Contacts Logs/Group Notes" is selected and the procedure is associated with a Daily/Per Diem billing type.
![]() When this option is checked and "Report Service Time" is selected, the following procedure options are disabled and made read-only: Aggregate Time (otherwise count contacts), Allow multiple services, and Create Weekly Invoice.
When this option is checked and "Report Service Time" is selected, the following procedure options are disabled and made read-only: Aggregate Time (otherwise count contacts), Allow multiple services, and Create Weekly Invoice.
![]() This procedure option is designed to work with a single note to invoice relationship, not multiple notes. If there are multiple notes attached to the procedures invoice, only the first note start and end time are used.
This procedure option is designed to work with a single note to invoice relationship, not multiple notes. If there are multiple notes attached to the procedures invoice, only the first note start and end time are used.
![]() The NTE data is assigned to the invoice when the invoice is posted to A/R.
The NTE data is assigned to the invoice when the invoice is posted to A/R.
![]() If a procedure using this option has a posted invoice associated with it, this option becomes disabled and read-only.
If a procedure using this option has a posted invoice associated with it, this option becomes disabled and read-only.
![]() Report NTE (Third Party Org Note) Segment in 837 - Click this checkbox to report the NTE segment in both the 837P or 837I files. Once checked, enter the associated NTE reference code within the Note Reference Code text box. Lastly, click one of the following corresponding radio buttons:
Report NTE (Third Party Org Note) Segment in 837 - Click this checkbox to report the NTE segment in both the 837P or 837I files. Once checked, enter the associated NTE reference code within the Note Reference Code text box. Lastly, click one of the following corresponding radio buttons:
Report Service Time - Select this option to report the start time and end time of the progress note or group note that created the invoice. This data will be reported as SVCSTIME(+2 blank spaces)note start and end time in military format; for example, SVCSTIME 1100-1200.
Report General Message - Select this option to report a general message each time the procedure is invoiced.
![]() NOTE: Please note the following regarding this procedure option:
NOTE: Please note the following regarding this procedure option:
![]() It is only available if the billable document type of "Services - Progress Notes/Contacts Logs/Group Notes" is selected and the procedure is associated with a Daily/Per Diem billing type.
It is only available if the billable document type of "Services - Progress Notes/Contacts Logs/Group Notes" is selected and the procedure is associated with a Daily/Per Diem billing type.
![]() When this option is checked and "Report Service Time" is selected, the following procedure options are disabled and made read-only: Aggregate Time (otherwise count contacts), Allow multiple services, and Create Weekly Invoice.
When this option is checked and "Report Service Time" is selected, the following procedure options are disabled and made read-only: Aggregate Time (otherwise count contacts), Allow multiple services, and Create Weekly Invoice.
![]() This procedure option is designed to work with a single note to invoice relationship, not multiple notes. If there are multiple notes attached to the procedures invoice, only the first note start and end time are used.
This procedure option is designed to work with a single note to invoice relationship, not multiple notes. If there are multiple notes attached to the procedures invoice, only the first note start and end time are used.
![]() The NTE data is assigned to the invoice when the invoice is posted to A/R.
The NTE data is assigned to the invoice when the invoice is posted to A/R.
![]() If a procedure using this option has a posted invoice associated with it, this option becomes disabled and read-only.
If a procedure using this option has a posted invoice associated with it, this option becomes disabled and read-only.
![]() Place of Service Code (837P)/Uniform Bill Type Code (837I) - Click the appropriate radio button to indicate how the procedure needs to report the POS/UBTC. Available options are:
Place of Service Code (837P)/Uniform Bill Type Code (837I) - Click the appropriate radio button to indicate how the procedure needs to report the POS/UBTC. Available options are:
Do Not Use - The default selection. Reports the data entered within the CMS Place of Service/Uniform Bill Type Code from the Program Billing Info page.
Progress/Group Notes Location POS Code - Reports a code based on the location selected within the note being billed, using the crosswalk provided here. (Note that if more than one note is used to generate an invoice for the procedure, the location of the first note written on that day is used.)
|
Selected Location |
POS Code |
|
None selected |
11 |
|
Equals "this program site" OR contains "Office" |
11 |
|
Contains "residence" or "home" |
12 |
|
Equals "school" |
03 |
|
Equals "emergency room" |
23 |
|
Equals "hospital" |
21 |
|
Equals "Jail" OR contains "correctional facility" |
09 |
|
Equals "Telehealth" OR contains "telehealth" |
02 |
|
Equals "Client Workplace" |
18 |
|
Contains "Residential Substance Abuse Facility" |
55 |
|
Contains "Homeless Shelter" |
04 |
|
Contains "Group Home" |
14 |
|
Contains "Temporary Lodging" |
16 |
|
Does not meet any of the above requirements |
99 |
Default Place of Service Code/Uniform Bill Type Code - Provides a text field where a default code can be entered for the procedure. If data is entered here it is used in place of the CMS Place of Service/Uniform Bill Type Code value entered in Program Billing Info.
![]() Staff Credentials Required - If applicable, click the checkbox(es) next to the credentials a provider must have in order to bill for this procedure. Any credentials set as required in this step must be assigned to the provider using the Credentials portion of the Human Resources module's Staff Information feature.
Staff Credentials Required - If applicable, click the checkbox(es) next to the credentials a provider must have in order to bill for this procedure. Any credentials set as required in this step must be assigned to the provider using the Credentials portion of the Human Resources module's Staff Information feature.
![]() TIP: If there are required credentials used in your agency that are not listed, or you do not see the option to record credentials, contact the Help Desk to have them added to the system.
TIP: If there are required credentials used in your agency that are not listed, or you do not see the option to record credentials, contact the Help Desk to have them added to the system.
![]() Primary Procedure or Add On Procedure or Required Condition to be Added to a Procedure - Click one of the procedure radio buttons to indicate whether this procedure is primary or add on.
Primary Procedure or Add On Procedure or Required Condition to be Added to a Procedure - Click one of the procedure radio buttons to indicate whether this procedure is primary or add on.
![]() NOTE: This option is available for Monthly and Daily/Per Diem billing types only, where clients are theoretically limited to one invoice per day or per month. In reality, both Monthly and Per Diem billing types allow for multiple invoices, with one primary invoice and sometimes multiple add-ons. For example, a "counseling session" could be the primary procedure, but if it is done in the client's home an additional procedure could be added on and more money could be collected for an "at home visit."
NOTE: This option is available for Monthly and Daily/Per Diem billing types only, where clients are theoretically limited to one invoice per day or per month. In reality, both Monthly and Per Diem billing types allow for multiple invoices, with one primary invoice and sometimes multiple add-ons. For example, a "counseling session" could be the primary procedure, but if it is done in the client's home an additional procedure could be added on and more money could be collected for an "at home visit."
![]() NOTE: If the billing type is Monthly, the Primary Procedure option will be listed as Primary Procedure (one per month/consumer) everywhere on the page, and the Add On Procedure option will be listed as Add On Procedure (multiple per month/consumer) everywhere on the page.
NOTE: If the billing type is Monthly, the Primary Procedure option will be listed as Primary Procedure (one per month/consumer) everywhere on the page, and the Add On Procedure option will be listed as Add On Procedure (multiple per month/consumer) everywhere on the page.
If the billing type is Daily/Per Diem, the Primary Procedure option will be listed as Primary Procedure (one per day/consumer) everywhere on the page, and the Add On Procedure option will be listed as Add On Procedure (Multiple per day/consumer) everywhere on the page.
If the procedure is an add-on procedure (Add on Procedure is selected), the following additional options are included on the page:
Procedure Order - In this text box enter a number from 0-99. The number entered here is used to determine which procedures are considered for billing first when the billing type/procedures are used to generate a batch. Please note, this setting is optional and is not needed in most billing configurations.
Create Invoice if ANY primary procedure or primary requirement is being billed or Create invoice if this primary procedure or primary requirement is being billed or Create if this primary procedure is NOT being billed - Select the appropriate radio button, and if necessary select the primary procedure in the corresponding checklist.
Create Invoice if no primary procedure is being billed - Click this checkbox to bill the add-on procedure with no primary procedure.
Require Plan or Review effective date OR service plan done date within _____ days prior to date of service, with _____ electronic signature - In the text box, enter the maximum number of days prior to the date of service that a plan or review must have been marked effective, OR a service plan must have been marked done, in order to make the procedure billable. If the plan, review, or service plan must be electronically signed in
![]() NOTE: If no days are entered this requirement will not apply. The option for electronic signatures on service plans only applies when this option is activated for the agency.
NOTE: If no days are entered this requirement will not apply. The option for electronic signatures on service plans only applies when this option is activated for the agency.
![]() TIP: If you create more than one primary procedure for a Per Diem billing type, the following rules apply:
TIP: If you create more than one primary procedure for a Per Diem billing type, the following rules apply:
![]() If both procedures are "face to face contacts counts," AWARDS will create an invoice only for the procedure with the higher rate if both procedures are provided to a single client on a given day.
If both procedures are "face to face contacts counts," AWARDS will create an invoice only for the procedure with the higher rate if both procedures are provided to a single client on a given day.
![]() If one procedure is "attendance hours" and the other procedure is a "face to face contacts count" billing unit requirement, then only the face to face contact procedure is invoices. To be able to create an invoice for both procedures, one of them needs to be changed to an add-on procedure.
If one procedure is "attendance hours" and the other procedure is a "face to face contacts count" billing unit requirement, then only the face to face contact procedure is invoices. To be able to create an invoice for both procedures, one of them needs to be changed to an add-on procedure.
![]() Use sliding scale percent - Click this checkbox if the rate to be charged for the procedure is a percentage of the procedure cost.
Use sliding scale percent - Click this checkbox if the rate to be charged for the procedure is a percentage of the procedure cost.
![]() TIP: This option is only recommended for "Self Pay" payers. If checked, a sliding scale rate for each client can be entered under "Insurance/Subsidized Payments Information" using the Entitlements module Certified Entitlements feature.
TIP: This option is only recommended for "Self Pay" payers. If checked, a sliding scale rate for each client can be entered under "Insurance/Subsidized Payments Information" using the Entitlements module Certified Entitlements feature.
![]() Transportation Locations - If Billable Documentation Type is set to "Services - Transportation," select the billable transportation locations for the procedure. These are the same locations that are seen when entering expected passengers data in the Transportation feature.
Transportation Locations - If Billable Documentation Type is set to "Services - Transportation," select the billable transportation locations for the procedure. These are the same locations that are seen when entering expected passengers data in the Transportation feature.
![]() TIP: At least one transportation location must be selected from the Pick Up and Drop Off lists.
TIP: At least one transportation location must be selected from the Pick Up and Drop Off lists.
![]() IMPORTANT! Which of the fields and options listed below you see will vary based on the combination of billing unit type and units of service requirements you previously selected. Not all fields/options will appear in all cases as documentation requirements will vary.
IMPORTANT! Which of the fields and options listed below you see will vary based on the combination of billing unit type and units of service requirements you previously selected. Not all fields/options will appear in all cases as documentation requirements will vary.
![]() Attendance Types - This set of checkboxes is available for use when the Billable Documentation Types option on the Billing Procedures Setup page (step 8) is set to "Reception Desk - Attendance/Group Activities." For Attendance Types, click one or both checkboxes to select where the billable attendance records can be found for the procedure: "Reception Desk - Attendance" or "Services - Group - Group Activities." If both options are selected, AWARDS will look for both types of records and if at least one is found the procedure requirement will be met. This procedure setting uses an OR statement and not an AND statement.
Attendance Types - This set of checkboxes is available for use when the Billable Documentation Types option on the Billing Procedures Setup page (step 8) is set to "Reception Desk - Attendance/Group Activities." For Attendance Types, click one or both checkboxes to select where the billable attendance records can be found for the procedure: "Reception Desk - Attendance" or "Services - Group - Group Activities." If both options are selected, AWARDS will look for both types of records and if at least one is found the procedure requirement will be met. This procedure setting uses an OR statement and not an AND statement.
![]() Additional Billable Events - if any of the following options are set to "Yes," then these events will count towards billing, regardless of which billable documentation type was selected on the previous page and regardless of any requirements set forth lower down on the page:
Additional Billable Events - if any of the following options are set to "Yes," then these events will count towards billing, regardless of which billable documentation type was selected on the previous page and regardless of any requirements set forth lower down on the page:
Invoice Calendar Appointments Marked as Kept? - Click this drop-down arrow and select "Yes" or "No" to indicate whether an appointment marked as kept on the AWARDS Calendar is sufficient documentation to bill, with or without corresponding documentation of contact (such as progress notes).
![]() TIP: Completed Medical Encounter Forms will also be counted as kept appointments when this option is set to "Yes."
TIP: Completed Medical Encounter Forms will also be counted as kept appointments when this option is set to "Yes."
Invoice Referral Interviews/Assessments? - Click this drop-down arrow and select "Yes" or "No" to indicate whether a referral interview scheduled and marked as held on the client's referral form or the AWARDS Calendar is sufficient documentation to bill, with or without corresponding documentation of contact (such as progress notes).
Invoice Charting Events Marked as Done? - Click this drop-down arrow and select "Yes" or "No" to indicate whether an event scheduled on the Charting Timetable and marked as complete counts as documentation used for billing purposes.
![]() TIP: If "Yes" is selected and you only want charting events to count as billable events, excluding progress and group notes, make sure that you uncheck the "Individual One-on-One" and "Group" checkboxes that appear further down on this page, as well as both the "Routine" and "Crisis" checkboxes that appear in the "Crisis?" field.
TIP: If "Yes" is selected and you only want charting events to count as billable events, excluding progress and group notes, make sure that you uncheck the "Individual One-on-One" and "Group" checkboxes that appear further down on this page, as well as both the "Routine" and "Crisis" checkboxes that appear in the "Crisis?" field.
List name/s of Charting Event/s - This is a list of charting events available for the program type selected on the first Billing Procedures Setup page. Click the checkbox next to each chart event that counts towards billing for this procedure.
![]() TIP: If no charting events are selected then all of the events listed will count towards billing.
TIP: If no charting events are selected then all of the events listed will count towards billing.
![]() Minimum # of days in program / Maximum # of days in program - If the number of days of program enrollment is the documentation requirement for billing, then in these fields type minimum and maximum days in program values to indicate the range within which a client's program days must fall for the procedure to be billable.
Minimum # of days in program / Maximum # of days in program - If the number of days of program enrollment is the documentation requirement for billing, then in these fields type minimum and maximum days in program values to indicate the range within which a client's program days must fall for the procedure to be billable.
![]() Minimum # of contacts / Maximum # of contacts and Billable Cap - If contact is the documentation requirement for billing then in these fields type minimum and maximum number of contacts values to indicate the range within which a client's number of contacts must fall for the procedure to be billable. If there is a maximum number of contacts entered in the corresponding Billable Cap field, the procedure will be billed if the number of contacts equals or exceeds that maximum.
Minimum # of contacts / Maximum # of contacts and Billable Cap - If contact is the documentation requirement for billing then in these fields type minimum and maximum number of contacts values to indicate the range within which a client's number of contacts must fall for the procedure to be billable. If there is a maximum number of contacts entered in the corresponding Billable Cap field, the procedure will be billed if the number of contacts equals or exceeds that maximum.
![]() Minimum # of aggregate hours / Maximum # of aggregate hours - If aggregated contact time is required for billing then in these fields type minimum and maximum number of aggregate hour values to indicate the range within which a client's hours must fall for the procedure to be billable.
Minimum # of aggregate hours / Maximum # of aggregate hours - If aggregated contact time is required for billing then in these fields type minimum and maximum number of aggregate hour values to indicate the range within which a client's hours must fall for the procedure to be billable.
![]() Minimum contact duration (in minutes) / Maximum contact duration (in minutes) and Billable Cap - If a contact must be of a minimum or maximum duration in order to be billable then in these fields type the minimum or maximum number of minutes a contact must be in order for the procedure to be billable. If there is a maximum contact duration entered in the corresponding Billable Cap field, the procedure will be billed if the contact duration equals or exceeds that maximum.
Minimum contact duration (in minutes) / Maximum contact duration (in minutes) and Billable Cap - If a contact must be of a minimum or maximum duration in order to be billable then in these fields type the minimum or maximum number of minutes a contact must be in order for the procedure to be billable. If there is a maximum contact duration entered in the corresponding Billable Cap field, the procedure will be billed if the contact duration equals or exceeds that maximum.
![]() Use Percentage of Service Time CPT/HCPCS & Modifier Code assignment - Click this checkbox to pair two procedures together and submit specific CPT/HCPCS & Modifier Codes as well as billing rates for those codes based on the percentage of time being billed for each procedure. When this option is checked, the following additional options are made available for data entry:
Use Percentage of Service Time CPT/HCPCS & Modifier Code assignment - Click this checkbox to pair two procedures together and submit specific CPT/HCPCS & Modifier Codes as well as billing rates for those codes based on the percentage of time being billed for each procedure. When this option is checked, the following additional options are made available for data entry:
Select a procedure to pair - Click this drop-down arrow select a procedure to pair to the procedure that is being configured. The selection list only shows procedures configured for the same billing type that also have this procedure option selected AND are not currently paired with another procedure.
CPT/HCPCS & Modifier Code (first text field on the left) - Enter the code and possible modifier(s) associated with the first percentage range for this procedure using the following format:
XXXXX (5 digit code)
XXXXX:XX (5 digit code + colon + 2 digit modifier with no spaces)
XXXXX:XX:XX (5 digit code + colon + 2 digit modifier + colon + 2 digit modifier with no spaces)
XXXXX:XX:XX:XX (5 digit code + colon + 2 digit modifier + colon + 2 digit modifier + colon + 2 digit modifier with no spaces)
XXXXX:XX:XX:XX:XX (5 digit code + colon + 2 digit modifier + colon + 2 digit modifier + colon + 2 digit modifier + colon + 2 digit modifier with no spaces)
Percentage Threshold - Enter the threshold (any number between 0 and 100) to be applied to the first set of codes being entered.
Include - Click this checkbox to include the Percentage Threshold in the range; for example, if you enter 100 for the threshold and click the "Include" checkbox, the range will be set as 100% to 100%.
CPT/HCPCS & Modifier Code (second text field on the right) - Enter the code and possible modifier(s) associated with the first percentage range for the procedure being paired using the following format:
XXXXX (5 digit code)
XXXXX:XX (5 digit code + colon + 2 digit modifier with no spaces)
XXXXX:XX:XX (5 digit code + colon + 2 digit modifier + colon + 2 digit modifier with no spaces)
XXXXX:XX:XX:XX (5 digit code + colon + 2 digit modifier + colon + 2 digit modifier + colon + 2 digit modifier with no spaces)
XXXXX:XX:XX:XX:XX (5 digit code + colon + 2 digit modifier + colon + 2 digit modifier + colon + 2 digit modifier + colon + 2 digit modifier with no spaces)
Once data is entered in all three fields, click Add new to add the codes and threshold range to the procedure.
![]() NOTE: Please note the following:
NOTE: Please note the following:
![]() When entering a percentage range in one procedure, the same range will automatically be added to the paired procedure.
When entering a percentage range in one procedure, the same range will automatically be added to the paired procedure.
![]() This procedure option is only shown for procedures when the following is true: a) the procedure is associated with a billing type where Daily Per/Diem has been selected as the Billing Unit Type, and b) the procedure has "Services - Progress Notes/Contacts Log/Group Notes" selected as the Billable Documentation Type.
This procedure option is only shown for procedures when the following is true: a) the procedure is associated with a billing type where Daily Per/Diem has been selected as the Billing Unit Type, and b) the procedure has "Services - Progress Notes/Contacts Log/Group Notes" selected as the Billable Documentation Type.
![]() The Edit Invoice Batch page for any invoices tied to a procedure using this option report the following information under "Procedure:" Rate/Procedure Code data (CPT/HCPCS @ Modifier Code data); for example, 12345 (67890:99)
The Edit Invoice Batch page for any invoices tied to a procedure using this option report the following information under "Procedure:" Rate/Procedure Code data (CPT/HCPCS @ Modifier Code data); for example, 12345 (67890:99)
![]() Billing rate entry can only happen for the ranges created with the procedure setting called "Use Percentage of Service Time CPT/HCPCS & Modifier Code assignment," not for the main Rate/Procedure code data entered on the first procedure configuration page.
Billing rate entry can only happen for the ranges created with the procedure setting called "Use Percentage of Service Time CPT/HCPCS & Modifier Code assignment," not for the main Rate/Procedure code data entered on the first procedure configuration page.
![]() The BillingBuilder ReportBuilder reports the "Range" CPT/HCPCS & Modifier code data associated with the procedures range being invoiced, not the CPT/HCPCS & Modifier Code data captured on the first procedure configuration page.
The BillingBuilder ReportBuilder reports the "Range" CPT/HCPCS & Modifier code data associated with the procedures range being invoiced, not the CPT/HCPCS & Modifier Code data captured on the first procedure configuration page.
![]() Minimum attendance time (in minutes) / Maximum attendance time (in minutes) - If an attendance record must be of a minimum or maximum duration in order to be billable then in these fields type the minimum or maximum number of minutes an attendance record must be in order for the procedure to be billable.
Minimum attendance time (in minutes) / Maximum attendance time (in minutes) - If an attendance record must be of a minimum or maximum duration in order to be billable then in these fields type the minimum or maximum number of minutes an attendance record must be in order for the procedure to be billable.
![]() Require Program Status - Click the checkbox next to the program status required to bill this procedure. (Available selections are based on the Program Type selection for this procedure as set in step 8.) If a program status is selected here, the consumer must have this same status assigned to him/her in the Program Status feature with a start date and end date that include the date of service being billed.
Require Program Status - Click the checkbox next to the program status required to bill this procedure. (Available selections are based on the Program Type selection for this procedure as set in step 8.) If a program status is selected here, the consumer must have this same status assigned to him/her in the Program Status feature with a start date and end date that include the date of service being billed.
![]() Visit Type (Reception Desk) - Available when the Billable Documentation Types option on the Billing Procedures Setup page (step 8) is set to "Reception Desk - Attendance/Group Activities" - AND - the Attendance Type option (earlier in the current step) is set to "Reception Desk - Attendance." (Available visit type selections are based on the Program Type for this procedure, as set in step 8.) If a visit type is selected here, the consumer's program attendance record from the Reception Desk must have this visit type selected.
Visit Type (Reception Desk) - Available when the Billable Documentation Types option on the Billing Procedures Setup page (step 8) is set to "Reception Desk - Attendance/Group Activities" - AND - the Attendance Type option (earlier in the current step) is set to "Reception Desk - Attendance." (Available visit type selections are based on the Program Type for this procedure, as set in step 8.) If a visit type is selected here, the consumer's program attendance record from the Reception Desk must have this visit type selected.
![]() Group Activity Types (Group Activities) - Available when the Billable Documentation Types option on the Billing Procedures Setup page (step 8) is set to "Reception Desk - Attendance/Group Activities" - AND - the Attendance Type option (earlier in the current step) is set to "Services - Group - Group Activities." (Available visit type selections are based on the Program Type for this procedure, as set in step 8.) If a group activity type is selected here, the same activity type must be assigned to the group activity attendance record that is automatically created when entering a note for a scheduled group.
Group Activity Types (Group Activities) - Available when the Billable Documentation Types option on the Billing Procedures Setup page (step 8) is set to "Reception Desk - Attendance/Group Activities" - AND - the Attendance Type option (earlier in the current step) is set to "Services - Group - Group Activities." (Available visit type selections are based on the Program Type for this procedure, as set in step 8.) If a group activity type is selected here, the same activity type must be assigned to the group activity attendance record that is automatically created when entering a note for a scheduled group.
![]() Minimum days of contact / Maximum days of contact - If the number of days of contact is the documentation requirement for billing then in these fields type the minimum and maximum number of days of contact values to indicate the range within which a client's contact days must fall for the procedure to be billable.
Minimum days of contact / Maximum days of contact - If the number of days of contact is the documentation requirement for billing then in these fields type the minimum and maximum number of days of contact values to indicate the range within which a client's contact days must fall for the procedure to be billable.
![]() Minimum # of attendance days / Maximum # of attendance days - If program attendance is the documentation requirement for billing, then in these fields type minimum and maximum attendance day values to indicate the range within which a client's attendance days must fall for the procedure to be billable.
Minimum # of attendance days / Maximum # of attendance days - If program attendance is the documentation requirement for billing, then in these fields type minimum and maximum attendance day values to indicate the range within which a client's attendance days must fall for the procedure to be billable.
![]() Progress Notes Face to Face - Click this drop-down arrow and select "Yes" or "No" to indicate whether encounters must be face to face in order for the procedure to be billable.
Progress Notes Face to Face - Click this drop-down arrow and select "Yes" or "No" to indicate whether encounters must be face to face in order for the procedure to be billable.
![]() Interactive Complexity - Click this drop-down and select "Yes" or "No" to indicate whether progress notes and/or group notes must have the interactive complexity drop-down set to "Yes" or "No" for the procedure to be billable.
Interactive Complexity - Click this drop-down and select "Yes" or "No" to indicate whether progress notes and/or group notes must have the interactive complexity drop-down set to "Yes" or "No" for the procedure to be billable.
![]() IMPORTANT! For this option to work correctly, the Interactive Complexity drop-down option must be turned on for both progress notes and group notes. To have this drop-down added for both note types, please contact the Help Desk for assistance.
IMPORTANT! For this option to work correctly, the Interactive Complexity drop-down option must be turned on for both progress notes and group notes. To have this drop-down added for both note types, please contact the Help Desk for assistance.
![]() Service Plan Linked Notes - Click this drop-down arrow and select "Yes" or "No" to indicate whether a service plan linked note must be documented to meet the requirements of this procedure. For more information on service plan linked progress notes, click here.
Service Plan Linked Notes - Click this drop-down arrow and select "Yes" or "No" to indicate whether a service plan linked note must be documented to meet the requirements of this procedure. For more information on service plan linked progress notes, click here.
![]() NOTE: This option was originally developed for CR and ACT Medicaid billing in New York State. It may not be a suitable setting for other programs/payers/states.
NOTE: This option was originally developed for CR and ACT Medicaid billing in New York State. It may not be a suitable setting for other programs/payers/states.
![]() Aggregate Time (otherwise count contacts) - Click this drop-down arrow and select "Yes" or "No" to indicate whether an aggregate count of hours should be used to determine whether a procedure is billable.
Aggregate Time (otherwise count contacts) - Click this drop-down arrow and select "Yes" or "No" to indicate whether an aggregate count of hours should be used to determine whether a procedure is billable.
![]() NOTE: If this option is set to "Yes," the number of contacts become irrelevant and the Minimum # of contacts, Maximum # of contacts, and Billable Cap fields are hidden from view.
NOTE: If this option is set to "Yes," the number of contacts become irrelevant and the Minimum # of contacts, Maximum # of contacts, and Billable Cap fields are hidden from view.
![]() Invoice Pre-admission Service Dates? - Click this drop-down arrow and select "Yes" or "No" to indicate whether services documented prior to the client's date of admission are billable.
Invoice Pre-admission Service Dates? - Click this drop-down arrow and select "Yes" or "No" to indicate whether services documented prior to the client's date of admission are billable.
![]() TIP: For example, if the client's Intake is processed and a progress note or group note is written, select "Yes" to count those services as billable.
TIP: For example, if the client's Intake is processed and a progress note or group note is written, select "Yes" to count those services as billable.
![]() Minimum # of aggregate hours and Maximum # of aggregate hours - If aggregate hours will be used to bill, then in these fields type the minimum or maximum number of aggregate hours a required in order for the procedure to be billable.
Minimum # of aggregate hours and Maximum # of aggregate hours - If aggregate hours will be used to bill, then in these fields type the minimum or maximum number of aggregate hours a required in order for the procedure to be billable.
![]() Service Types - Click the checkbox next to each service type applicable for billing in relation to this procedure. The list of service types available here is based on the program type selected on the first Billing Procedures Setup page.
Service Types - Click the checkbox next to each service type applicable for billing in relation to this procedure. The list of service types available here is based on the program type selected on the first Billing Procedures Setup page.
![]() TIP: If no billable service types are selected then all of the service types listed will count towards billing.
TIP: If no billable service types are selected then all of the service types listed will count towards billing.
![]() Progress Note Types - Click the checkbox next to each progress note type applicable for billing in relation to this procedure.
Progress Note Types - Click the checkbox next to each progress note type applicable for billing in relation to this procedure.
![]() TIP: If no progress note types are selected then all of the note types listed will count towards billing.
TIP: If no progress note types are selected then all of the note types listed will count towards billing.
![]() Ratio - Click the checkbox next to each ratio option that is applicable for billing in relation to this procedure, based on progress notes.
Ratio - Click the checkbox next to each ratio option that is applicable for billing in relation to this procedure, based on progress notes.
![]() TIP: If you do not currently see this option and would like to have it turned on for use when billing based on progress notes, please contact the Help Desk for assistance.
TIP: If you do not currently see this option and would like to have it turned on for use when billing based on progress notes, please contact the Help Desk for assistance.
![]() NOTE: This option is only available if the billable document type of "Services - Progress Notes/Contacts Logs/Group Notes" is selected, and the procedure is associated with a "Daily/Per Diem" billing type.
NOTE: This option is only available if the billable document type of "Services - Progress Notes/Contacts Logs/Group Notes" is selected, and the procedure is associated with a "Daily/Per Diem" billing type.
![]() NOTE: The label and checkbox options may vary based on the program type selected on the first page of the procedure configuration process.
NOTE: The label and checkbox options may vary based on the program type selected on the first page of the procedure configuration process.
![]() Progress / Group Note Writer - Click one of the following buttons to set a note writer NPI requirement for the procedure to be invoiced:
Progress / Group Note Writer - Click one of the following buttons to set a note writer NPI requirement for the procedure to be invoiced:
No NPI Requirement - The default selection. When selected the procedure can be invoiced whether or not the note writer has an NPI under Credentials in his/her Staff Information record.
Require NPI - When selected the procedure can only be invoiced if the note writer has an NPI under Credentials in his/her Staff Information record. When selecting this radio button you can also select a specific staff member from the corresponding drop-down. If a staff member is selected, the procedure is only billable when that staff member documents a group or progress note. If no staff member is selected, any staff member with an NPI is billable.
Require No NPI / Send Non-Covered Amount in 837 - When selected the procedure can be invoiced only if the note writer does NOT have an NPI under Credentials in his/her Staff Information record. In addition to setting this requirement to invoice the procedure, choosing this option results in the 837 claim file including the Non-Covered data segment AMT*A8.
![]() TIP: The AMT*A8 segment will be reported only if this is option is set for a procedure where the payer's name includes "Medicaid," and the consumer has both a "Medicare" payer listed as primary, and a "Medicaid" payer listed as secondary using the coordination of benefits setting in the client's entitlement record.
TIP: The AMT*A8 segment will be reported only if this is option is set for a procedure where the payer's name includes "Medicaid," and the consumer has both a "Medicare" payer listed as primary, and a "Medicaid" payer listed as secondary using the coordination of benefits setting in the client's entitlement record.
Additionally, because the non-covered amount is reported at the claim level (loop 2320) for an invoice, it is suggested that this option only be used for single procedure invoices or multi-line invoices where all procedures are set to report this data.
![]() Progress/Group Note Location - If the procedure must take place in a specific location in order to be billable, click this drop-down arrow and select the appropriate location.
Progress/Group Note Location - If the procedure must take place in a specific location in order to be billable, click this drop-down arrow and select the appropriate location.
![]() TIP: If no locations are selected then all of the locations listed will count towards billing.
TIP: If no locations are selected then all of the locations listed will count towards billing.
![]() Progress Notes/Contact Logs and Group Notes - By default both individual one-on-one and group contacts are billable. Uncheck either of these checkboxes as necessary to indicate that only individual contacts or only group contacts are billable for this procedure.
Progress Notes/Contact Logs and Group Notes - By default both individual one-on-one and group contacts are billable. Uncheck either of these checkboxes as necessary to indicate that only individual contacts or only group contacts are billable for this procedure.
![]() Require Electronically Signed Notes - Check this checkbox to require that a progress note be electronically signed before it can be used to generate an invoice.
Require Electronically Signed Notes - Check this checkbox to require that a progress note be electronically signed before it can be used to generate an invoice.
![]() NOTE: This checkbox is automatically selected when the EVV Procedure? option is checked off; however, it can be de-selected if needed.
NOTE: This checkbox is automatically selected when the EVV Procedure? option is checked off; however, it can be de-selected if needed.
![]() Group Note Activity Types - If a billable group needs to be a specific group activity type, check the checkbox(es) next to all applicable group activity types listed on this checklist.
Group Note Activity Types - If a billable group needs to be a specific group activity type, check the checkbox(es) next to all applicable group activity types listed on this checklist.
![]() Minimum Number of Consumers in the Group/Maximum Number of Consumers in the Group - Enter the minimum and maximum number of consumers needed in a group note for the procedure to be billable.
Minimum Number of Consumers in the Group/Maximum Number of Consumers in the Group - Enter the minimum and maximum number of consumers needed in a group note for the procedure to be billable.
![]() Allow Multiple Services - For per-diem billing click this checkbox to allow for billing more than one service in a given invoice for one day. For example, if there are five face-to-face contacts in a given day and this option is checked, then AWARDS will create one invoice which will include services for five face-to-face contacts.
Allow Multiple Services - For per-diem billing click this checkbox to allow for billing more than one service in a given invoice for one day. For example, if there are five face-to-face contacts in a given day and this option is checked, then AWARDS will create one invoice which will include services for five face-to-face contacts.
![]() Telehealth (Group Notes) - If necessary, click this drop-down arrow and select "Yes" or "No" to set this procedure to bill based on whether the Telehealth checkbox is selected in the group note. When "Yes" is selected here the Telehealth group note option must be checked off. When "No" is selected here the Telehealth group note option must be unselected. By default this drop-down selection is set to blank, allowing for both selected and unselected Telehealth values in the group note to be billable for the procedure.
Telehealth (Group Notes) - If necessary, click this drop-down arrow and select "Yes" or "No" to set this procedure to bill based on whether the Telehealth checkbox is selected in the group note. When "Yes" is selected here the Telehealth group note option must be checked off. When "No" is selected here the Telehealth group note option must be unselected. By default this drop-down selection is set to blank, allowing for both selected and unselected Telehealth values in the group note to be billable for the procedure.
![]() TIP: If you do not currently see this option and would like to have it turned on for use when billing based on group notes, please contact the Help Desk for assistance.
TIP: If you do not currently see this option and would like to have it turned on for use when billing based on group notes, please contact the Help Desk for assistance.
![]() Minimum Consumer Age and Maximum Consumer Age - In these fields type, if applicable, minimum and maximum age values to indicate the range within which a client's age must fall in order for the procedure to be billable. The client's age is calculated based on his or her date of birth.
Minimum Consumer Age and Maximum Consumer Age - In these fields type, if applicable, minimum and maximum age values to indicate the range within which a client's age must fall in order for the procedure to be billable. The client's age is calculated based on his or her date of birth.
![]() Minimum of GAF and Maximum of GAF - In these fields type, if applicable, minimum and maximum GAF scores to indicate the range within which a client's GAF score must fall in order for the procedure to be billable. The client's GAF Score is entered in the Diagnoses section of the face sheet or using the Medical module Diagnoses feature.
Minimum of GAF and Maximum of GAF - In these fields type, if applicable, minimum and maximum GAF scores to indicate the range within which a client's GAF score must fall in order for the procedure to be billable. The client's GAF Score is entered in the Diagnoses section of the face sheet or using the Medical module Diagnoses feature.
![]() Progress Note Crisis and/or Routine - By default both crisis and routine contacts are billable. Uncheck either of these checkboxes as necessary to indicate the requirements should be otherwise. The routine/crisis setting is found on individual progress notes.
Progress Note Crisis and/or Routine - By default both crisis and routine contacts are billable. Uncheck either of these checkboxes as necessary to indicate the requirements should be otherwise. The routine/crisis setting is found on individual progress notes.
![]() Documentation Start Time Begin and Documentation Start Time End - If an encounter must be held during a particular time of the day then set the start and end times within which the encounter must be held in order to be billable.
Documentation Start Time Begin and Documentation Start Time End - If an encounter must be held during a particular time of the day then set the start and end times within which the encounter must be held in order to be billable.
![]() Count by Unit of Service - Click this checkbox if billing at your agency is done by units of service, and enter the corresponding formula in the 1 unit = _____ minutes field.
Count by Unit of Service - Click this checkbox if billing at your agency is done by units of service, and enter the corresponding formula in the 1 unit = _____ minutes field.
![]() TIP: If billing at your agency is done by units of service, the contact time with a client is added together and then divided into units of service of a particular length. For example, if the total contact time with a client is 60 minutes and the Unit of Service is 15 minutes, then 4 units of service will be counted for the given billing type.
TIP: If billing at your agency is done by units of service, the contact time with a client is added together and then divided into units of service of a particular length. For example, if the total contact time with a client is 60 minutes and the Unit of Service is 15 minutes, then 4 units of service will be counted for the given billing type.
![]() TIP: If there is more than one contact (progress note or group note) for a client in a Per Diem billing type, then all contacts times will be aggregated and then divided into units of service of a particular length as described above.
TIP: If there is more than one contact (progress note or group note) for a client in a Per Diem billing type, then all contacts times will be aggregated and then divided into units of service of a particular length as described above.
![]() Service Units of Measure - Click the Calculate Units Using drop-down and make a selection to indicate how the procedure will calculate invoice units. Available options are:
Service Units of Measure - Click the Calculate Units Using drop-down and make a selection to indicate how the procedure will calculate invoice units. Available options are:
1 Unit Per Procedure - The default value. If selected, the procedure will always invoice 1 units of service.
Duration - If selected, the procedure will calculate service units based on the duration of service(s) and the following options are offered:
1 unit of measure = ___ minutes - Enter the number of minutes that define a unit of measure, using decimals if needed.
Count ____ or More Remaining Minutes as Whole Units of Measure - Click this radio button to count remaining minutes as another full unit of measure. If the field is left blank, any minutes above the unit of measure will be viewed as a full unit. If a number of minutes is entered in the field, AWARDS will round up if that number of minutes is reached or passed.
Apply Rounding to Units of Service Remainder - Click this radio button to round the invoice units to the nearest whole number.
Apply Rounding to Units of Measure Remainder - Click this radio button to round the invoice units to the nearest tenth of a unit.
Require full units of measure to calculate units of service - Click this radio button to require full units of measure to bill service units.
Minutes Deduction - Enter a value in this field if appropriate. The value specified will be used to deduct a number of minutes from the total billable service duration when calculating service/invoice units. For example, if the total billable service duration is 30 minutes, and 5 is entered in the Minutes Deduction field, the procedure would calculate service/invoice units using 25 minutes and not 30 minutes.
First calculate the units and then add all of the units together - Click this checkbox to aggregate the units from each individual service first, and then sum the units together when multiple services are billed using the same procedure code for a consumer/day.
![]() TIP: For example, if the function is set to "Require fill units of measure to calculate units of service" with 7.5 minutes = 1 unit of measure = 1 unit of service, then a 20 minute contact time will be 2 units of service. If the function is set to "Count Remaining Minutes as Whole Units" with the same settings, then a 20 minute contact time will be 3 units of service.
TIP: For example, if the function is set to "Require fill units of measure to calculate units of service" with 7.5 minutes = 1 unit of measure = 1 unit of service, then a 20 minute contact time will be 2 units of service. If the function is set to "Count Remaining Minutes as Whole Units" with the same settings, then a 20 minute contact time will be 3 units of service.
The invoice amount for units of service will be calculated using the following formula:
(Billing Rate) x (# of units of measure contained in the contact time, rounded up or down as configured) / (# of units of measure that define 1 unit of service)
For example, if 1 unit of measure = 7.5 minutes, and 2 units of measure = 1 unit of service, and the billing rate for the procedure is $50, the following formula would apply for a progress note of 15 minutes: 50 x 2 /2 = $50.
If there is more than one contact (progress note or group note) for a client in a Per Diem billing type, then all contact times will be aggregated and then divided into units of measure of a particular length as described above.
Custom Unit Type - If selected, the procedure will calculate service units based on miles entered within the Mileage field for progress notes, and the following options are offered:
![]() NOTE: This option is only available if the program type selected on the first screen of configuring a procedure has this drop-down activated.
NOTE: This option is only available if the program type selected on the first screen of configuring a procedure has this drop-down activated.
1 unit = ____ [unit type] - Enter the number of units that define a unit of measure, using decimals if needed, and then click the corresponding drop-down arrow and select the custom unit type being utilized. This drop-down list is populated with selections defined with the ListBuilder's "Progress Note Unit Types" record.
Maximum Count of Billable Units - In this field enter the maximum number of units of the custom type that are billable for this procedure. Both whole numbers and decimal values are allowed. If this field is left blank no cap is applied and a single progress note can be used to bill as many units as appropriate. If a value greater than 0 is specified, any progress notes that are billed using this procedure will only bill up to this number of units. If the progress note has more units than the maximum, those units remain on the progress note but are not billed when an invoice is generated.
Apply Rounding Down - Click this radio button to always round service units down.
Apply Rounding Up - Click this radio button to always round service units up.
Apply Rounding Natural - Click this radio button to round service units naturally (round down if closer to the lesser unit or up if closer to the higher unit).
Count ____ Remaining # of units as Whole Units of Measure - Click this radio button to count remaining # of units as another full unit of measure. If the field is left blank, any # of units above the unit of measure will be viewed as a full unit. If a number of units is entered in the field, AWARDS will round up if that number of units is reached or passed.
![]() Create Weekly Invoice - Only available for Daily/Per Diem and Fee for Service billing types. Click this checkbox to create one invoice per week per consumer for the selected procedure, based on all documentation meeting the requirements of the procedure. All requirements are considered over the course of a week (7 days), not a single day. When this option is used, the voice date on the Edit Invoice Batch page will be the end of the 7 day period. Additionally, the service date reported in the 837 claim file and the HCFA-1500 will be the full range of the 7 day period.
Create Weekly Invoice - Only available for Daily/Per Diem and Fee for Service billing types. Click this checkbox to create one invoice per week per consumer for the selected procedure, based on all documentation meeting the requirements of the procedure. All requirements are considered over the course of a week (7 days), not a single day. When this option is used, the voice date on the Edit Invoice Batch page will be the end of the 7 day period. Additionally, the service date reported in the 837 claim file and the HCFA-1500 will be the full range of the 7 day period.
![]() IMPORTANT! When this option is selected, please ensure that within the Maximum number of invoices per week option, Invoices is set to "1," and that the day the week starts has been indicated using the Week begins drop-down.
IMPORTANT! When this option is selected, please ensure that within the Maximum number of invoices per week option, Invoices is set to "1," and that the day the week starts has been indicated using the Week begins drop-down.
![]() Send exact service date range in 837 - Click this checkbox to send the actual start and end dates of the services data in the 837 file rather than the default week start and end dates.
Send exact service date range in 837 - Click this checkbox to send the actual start and end dates of the services data in the 837 file rather than the default week start and end dates.
Invoices - Indicate whether there is a maximum number of invoices for the procedure that can be generated per week by entering an integer in the Invoices field, and then indicate which day of the week should be used to calculate the start of the week by selecting it from the corresponding drop-down list.
Units - Indicate whether there is a maximum number of units for the procedure that can be generated per week by entering an integer in the Units field, and then indicate which day of the week should be used to calculate the start of the week by selecting it from the corresponding drop-down list.
![]() Require specific weekdays - Select the weekdays on which the procedure is billable.
Require specific weekdays - Select the weekdays on which the procedure is billable.
![]() TIP: This procedure option is only applied to Daily/Per Diem billing type procedures.
TIP: This procedure option is only applied to Daily/Per Diem billing type procedures.
![]() Measurement Code (SV103) - Click one of the following radio buttons to report the appropriate measurement code within the SV2 segment of the 837 file.
Measurement Code (SV103) - Click one of the following radio buttons to report the appropriate measurement code within the SV2 segment of the 837 file.
![]() NOTE: This option is only displayed in the Billing Unit Type on the Edit Billing Types page is "Daily/Per Diem" and the Billable Documentation Type on the Billing Procedure Setup page has been set to "Housing - Nightly Absences."
NOTE: This option is only displayed in the Billing Unit Type on the Edit Billing Types page is "Daily/Per Diem" and the Billable Documentation Type on the Billing Procedure Setup page has been set to "Housing - Nightly Absences."
Units (UN) - The default selection. Select this option to report "UN" in SV2-04.
Days (DA) - Select this option to report "DA" in SV2-04.
Minutes (MJ) - Select this option to report "MJ" in SV2-04.
![]() Program division enrollment is required - If there are program divisions set up for programs in the program billing group, a procedure can require program division enrollment in order to be billable. Check this checkbox to activate this billing requirement.
Program division enrollment is required - If there are program divisions set up for programs in the program billing group, a procedure can require program division enrollment in order to be billable. Check this checkbox to activate this billing requirement.
![]() NOTE: This option is only available for agencies that have program divisions set up within the Services - Group module's Group Schedule Setup feature.
NOTE: This option is only available for agencies that have program divisions set up within the Services - Group module's Group Schedule Setup feature.
![]() NOTE: This procedure setting is not used as a billing requirement, and it does not affect data reported in the 837 claim file or paper claim formats.
NOTE: This procedure setting is not used as a billing requirement, and it does not affect data reported in the 837 claim file or paper claim formats.
The process of configuring new procedures is now complete.
![]() TIP: If it is later necessary to update or delete a procedure, complete steps 1 through 5 above, select the billing type in question, and then click EDIT PROCEDURES. On the page that follows, select the procedure and click UPDATE or DELETE as appropriate. Keep in mind:
TIP: If it is later necessary to update or delete a procedure, complete steps 1 through 5 above, select the billing type in question, and then click EDIT PROCEDURES. On the page that follows, select the procedure and click UPDATE or DELETE as appropriate. Keep in mind:
![]() When updating - If changes are made, be sure to click both UPDATE & IDENTIFY UNITS OF SERVICE on the Billing Procedures Setup page, and UPDATE & CONFIRM PROCEDURE SETUP on the Identify Units of Service page to have those changes applied.
When updating - If changes are made, be sure to click both UPDATE & IDENTIFY UNITS OF SERVICE on the Billing Procedures Setup page, and UPDATE & CONFIRM PROCEDURE SETUP on the Identify Units of Service page to have those changes applied.
![]() When deleting - The deletion will occur as soon as DELETE is clicked. There is no confirmation page, and once deleted a procedure cannot be restored. Procedures can only be deleted when there are no invoices created for that procedure.
When deleting - The deletion will occur as soon as DELETE is clicked. There is no confirmation page, and once deleted a procedure cannot be restored. Procedures can only be deleted when there are no invoices created for that procedure.
AWARDS Hard Coded Billing Types / Procedures
If you are configuring billing for one of the following three hard coded billing types (PROS, ACT, CR), the procedure configuration page includes a very limited number of user inputs as the billing rules/requirements are not configurable in AWARDS.
If a hard coded PROS procedure is selected, the following options are available:
![]() Authorization is required - Click this checkbox if the payer requires prior authorization for this procedure.
Authorization is required - Click this checkbox if the payer requires prior authorization for this procedure.
![]() TIP: If authorization is required, a client's authorization information is entered in the "BillingBuilder Insurance Authorizations" section of the Certified Entitlements feature, accessible from within the Entitlements module or from the client's face sheet.
TIP: If authorization is required, a client's authorization information is entered in the "BillingBuilder Insurance Authorizations" section of the Certified Entitlements feature, accessible from within the Entitlements module or from the client's face sheet.
If a billing procedure is configured to require authorization, then AWARDS will not bill for a client for that procedure unless there is a current authorization record found in that client's entitlements.
If a hard coded ACT procedure is selected, the following options are available:
![]() Authorization is required - Click this checkbox if the payer requires prior authorization for this procedure.
Authorization is required - Click this checkbox if the payer requires prior authorization for this procedure.
![]() TIP: If authorization is required, a client's authorization information is entered in the "BillingBuilder Insurance Authorizations" section of the Certified Entitlements feature, accessible from within the Entitlements module or from the client's face sheet.
TIP: If authorization is required, a client's authorization information is entered in the "BillingBuilder Insurance Authorizations" section of the Certified Entitlements feature, accessible from within the Entitlements module or from the client's face sheet.
If a billing procedure is configured to require authorization, then AWARDS will not bill for a client for that procedure unless there is a current authorization record found in that client's entitlements.
If a hard coded CR procedure is selected, the following options are available:
![]() Billing Provider NPI - In this field, enter the NPI to be reported as the billing provider NPI in the 837 claim file in place of the Billing Provider NPI on the Program Billing Groups page.
Billing Provider NPI - In this field, enter the NPI to be reported as the billing provider NPI in the 837 claim file in place of the Billing Provider NPI on the Program Billing Groups page.
![]() Billing Provider Address - In this field, enter the billing provider address to be reported as the billing provider address in the 837 claim file in place of the Sender Address on the Program Billing Groups page.
Billing Provider Address - In this field, enter the billing provider address to be reported as the billing provider address in the 837 claim file in place of the Sender Address on the Program Billing Groups page.
https://demodb.footholdtechnology.com/help/?11427