|   |
|   |
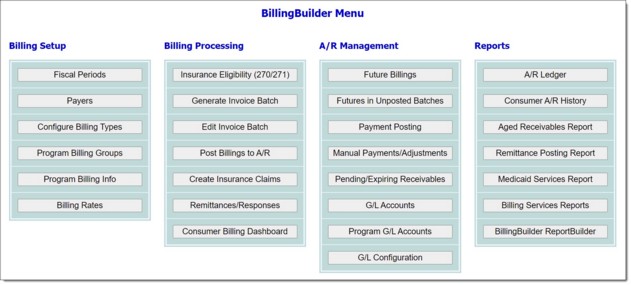
Every program that bills must have program billing information entered for it. That information, which is entered in step 6 of the setup process, consists of specific data required for electronic claim files or paper invoice forms.
![]() NOTE: Programs can belong to only one program billing group at a time.
NOTE: Programs can belong to only one program billing group at a time.
To configure a program's billing information, complete the following steps:
![]() IMPORTANT! Each program/payer combination can only belong to one program billing group at a time.
IMPORTANT! Each program/payer combination can only belong to one program billing group at a time.
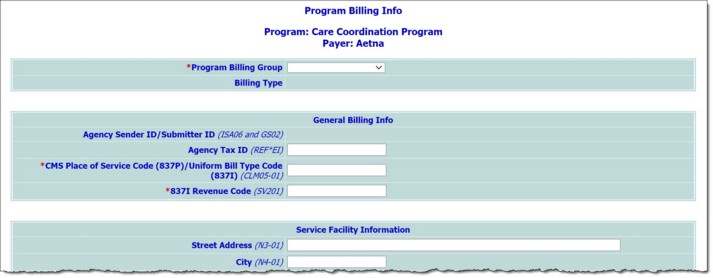
To enter or update program billing information for the selected program and payer combination, configure the fields and options on this page as follows:
![]() Program Billing Group - Click this drop-down arrow and select the program billing group with which this program should be associated. When a selection is made the page is automatically refreshed and values for the selected group are dropped into the Agency Sender ID/Submitter ID and Agency Tax ID fields (detailed below) if they were filled out during the configure billing type process.
Program Billing Group - Click this drop-down arrow and select the program billing group with which this program should be associated. When a selection is made the page is automatically refreshed and values for the selected group are dropped into the Agency Sender ID/Submitter ID and Agency Tax ID fields (detailed below) if they were filled out during the configure billing type process.
General Billing Info
![]() Agency Sender ID/Submitter ID - A read-only value displaying the Agency Sender ID/Submitter ID entered during program billing group configuration. The Sender Code entered there is also displayed here. This information can only be changed from within the Program Billing Groups feature.
Agency Sender ID/Submitter ID - A read-only value displaying the Agency Sender ID/Submitter ID entered during program billing group configuration. The Sender Code entered there is also displayed here. This information can only be changed from within the Program Billing Groups feature.
![]() NOTE: Defaults to the value entered for the associated billing type, if available for that type.
NOTE: Defaults to the value entered for the associated billing type, if available for that type.
![]() Agency Tax ID - In this field, type the agency's tax ID. When entering the ID, omit the dash after the second character.
Agency Tax ID - In this field, type the agency's tax ID. When entering the ID, omit the dash after the second character.
![]() NOTE: Defaults to the value entered for the associated billing type, if available for that type.
NOTE: Defaults to the value entered for the associated billing type, if available for that type.
![]() CMS Place of Service Code (837P)/Uniform Bill Type Code (837I) - For 837P billing types, enter the CMS place of service code in this field. For 837I billing types, enter the NUBC code. If the payer for this billing type is self-pay, enter "0" in this field.
CMS Place of Service Code (837P)/Uniform Bill Type Code (837I) - For 837P billing types, enter the CMS place of service code in this field. For 837I billing types, enter the NUBC code. If the payer for this billing type is self-pay, enter "0" in this field.
![]() 837I Revenue Code - In this field, type the four-digit 837 institutional revenue code. If this program billing info record is being used to generate an 837P (professional) claim file, "N/A" can be entered here.
837I Revenue Code - In this field, type the four-digit 837 institutional revenue code. If this program billing info record is being used to generate an 837P (professional) claim file, "N/A" can be entered here.
Service Facility Information
The information in this section of the billing info page is used as the service facility information when the associated payer has the Report Service Facility Info in 837 option checked off and the procedure being invoiced as the Use Program Billing Info option selected for the "Service Facility Info for 837" setting.
![]() Street Address - In this field, type the service facility street address for this program billing info record.
Street Address - In this field, type the service facility street address for this program billing info record.
![]() City - In this field, type the service facility city for this program billing info record.
City - In this field, type the service facility city for this program billing info record.
![]() Street - Click this drop-down arrow and select the service facility state for this program billing info record.
Street - Click this drop-down arrow and select the service facility state for this program billing info record.
![]() Zip Code - In this field, type the service facility code for this program billing info record.
Zip Code - In this field, type the service facility code for this program billing info record.
![]() NPI - In this field, type the service facility NPI for this program billing info record.
NPI - In this field, type the service facility NPI for this program billing info record.
![]() Secondary ID, 837 ID Qualifier - In this field, type the service facility secondary ID and associated 837 ID qualifier for this program billing info record.
Secondary ID, 837 ID Qualifier - In this field, type the service facility secondary ID and associated 837 ID qualifier for this program billing info record.
![]() TIP: To report the secondary ID/qualifier, the Payers page needs to have the Report Service Facility Secondary ID option selected.
TIP: To report the secondary ID/qualifier, the Payers page needs to have the Report Service Facility Secondary ID option selected.
Default Rendering/Attending Provider Info for Program
The read-only information displayed in this section of the billing info page is used as the Rendering/Attending NPI for an invoice on the Edit Invoice Batch page when the note writer does not have an NPI entered for them under Human Resources > Staff Information > Credentials tab > National Provider Identifier AND when the procedure being invoiced does not have data entered within the Incident To fields.
Retaining this history allows AWARDS to always report the correct NPI based on the date of service being invoiced. If no records are entered or in effect at that time, the Rendering/Attending NPI field will be blank on the Edit Invoice Batch screen.
If it is necessary to add to or edit this information you will have the opportunity to do so in step 9, below.
Atypical Billing Options
The information in this section of the billing info page is used if the program billing info record needs to create an atypical 837 claim file. Typically, atypical 837 claim files report an MPI (Medicaid Provider ID) and not an NPI (National Provider ID).
![]() Medicaid Provider ID - If billing an atypical 837 file, enter the agency/program's Medicaid Provider ID in this field.
Medicaid Provider ID - If billing an atypical 837 file, enter the agency/program's Medicaid Provider ID in this field.
![]() Locator Code - If billing an atypical 837 file, enter the agency/program's locator code in this field.
Locator Code - If billing an atypical 837 file, enter the agency/program's locator code in this field.
Additional Non Claim Data
If applicable, enter the information below. Please note that the information below is NOT used in the 837I or 837P claim files.
![]() Specialty Code - In this field, type the program's specialty code.
Specialty Code - In this field, type the program's specialty code.
![]() Category of Service - In this field, type the program's category of service.
Category of Service - In this field, type the program's category of service.
![]()
![]() Add a default rendering/attending provider information record - To do so, click the add new icon from the action bar above the records table. A new data entry page is displayed. Configure the fields and options on this page as necessary, and then click Save.
Add a default rendering/attending provider information record - To do so, click the add new icon from the action bar above the records table. A new data entry page is displayed. Configure the fields and options on this page as necessary, and then click Save.
![]() First Name - In this field, type the default rendering/attending provider's first name for this program billing info record.
First Name - In this field, type the default rendering/attending provider's first name for this program billing info record.
![]() Last Name - In this field, type the default rendering/attending provider's last name for this program billing info record.
Last Name - In this field, type the default rendering/attending provider's last name for this program billing info record.
![]() NPI - In this field, type the default rendering/attending provider's NPI for this program billing info record.
NPI - In this field, type the default rendering/attending provider's NPI for this program billing info record.
![]() Taxonomy Code - In this field, type the default rendering/attending provider's taxonomy code for this program billing info record.
Taxonomy Code - In this field, type the default rendering/attending provider's taxonomy code for this program billing info record.
![]() Secondary ID, 837 ID Qualifier - In this field, type the default rendering/attending provider's secondary ID and associated 837 ID qualifier for this program billing info record.
Secondary ID, 837 ID Qualifier - In this field, type the default rendering/attending provider's secondary ID and associated 837 ID qualifier for this program billing info record.
![]() TIP: To report the taxonomy code and/or secondary ID/qualifier, the Payers page needs to have one or both of the following options selected: Report Rendering/Attending Provider Taxonomy Code in 837 and/or Report Rendering/Attending Provider Secondary ID in 837.
TIP: To report the taxonomy code and/or secondary ID/qualifier, the Payers page needs to have one or both of the following options selected: Report Rendering/Attending Provider Taxonomy Code in 837 and/or Report Rendering/Attending Provider Secondary ID in 837.
![]()
![]() Update an existing default rendering/attending provider information record - To do so, click the record to be updated, or click the checkbox to the left of that record and then click the edit icon from the action bar above the records table. The data entry page is displayed. Make changes to the information on this page as needed, and then click Save. The record is saved, and a confirmation page is displayed.
Update an existing default rendering/attending provider information record - To do so, click the record to be updated, or click the checkbox to the left of that record and then click the edit icon from the action bar above the records table. The data entry page is displayed. Make changes to the information on this page as needed, and then click Save. The record is saved, and a confirmation page is displayed.
![]()
![]() View or print an existing default rendering/attending provider information record - To do so, click the checkbox to the left the record to be viewed/printed, and then click the view icon from the action bar above the records table. A read-only version of the record is displayed and can be printed as needed using your browser's print option.
View or print an existing default rendering/attending provider information record - To do so, click the checkbox to the left the record to be viewed/printed, and then click the view icon from the action bar above the records table. A read-only version of the record is displayed and can be printed as needed using your browser's print option.
![]()
![]() Delete an existing default rendering/attending provider information record - To do so, click the checkbox(es) to the left of the record(s) to be deleted, and then click the delete icon from the action bar above the records table. A confirmation message is displayed. Click OK to proceed with the deletion. The selected record(s) are deleted and the updated index is displayed.
Delete an existing default rendering/attending provider information record - To do so, click the checkbox(es) to the left of the record(s) to be deleted, and then click the delete icon from the action bar above the records table. A confirmation message is displayed. Click OK to proceed with the deletion. The selected record(s) are deleted and the updated index is displayed.
When all data entry is complete, click Return to Program Billing Info to continue the billing information configuration process.
The process of configuring program billing information is now complete.
![]() TIP: If it is later necessary to update a program's billing information, use the same procedure outlined above.
TIP: If it is later necessary to update a program's billing information, use the same procedure outlined above.
https://demodb.footholdtechnology.com/help/?11428