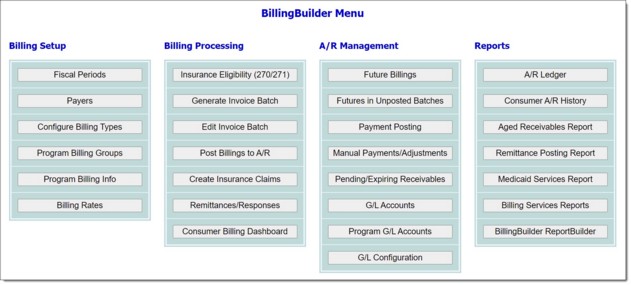
|   |
|   |
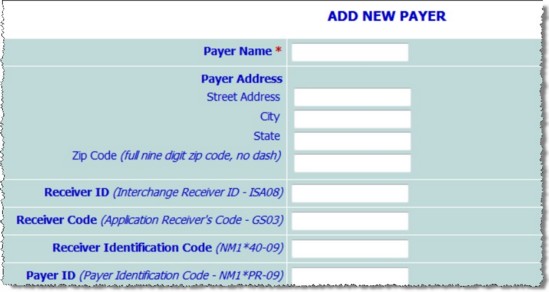
The second step in the BillingBuilder setup process is configuring payers. Payers include Medicaid, Medicare, private insurances, self-paying clients, or any other entity from which your programs receive payments for services provided.
To configure a new payer, complete the following steps:
![]() Payer Name - In this field, type the name of the payer; for example, "Medicaid." Be sure to enter the name carefully, as once saved it cannot be changed.
Payer Name - In this field, type the name of the payer; for example, "Medicaid." Be sure to enter the name carefully, as once saved it cannot be changed.
![]() TIP: If the payer is actually the client receiving the service, the "Self-Pay" payer should be used.
TIP: If the payer is actually the client receiving the service, the "Self-Pay" payer should be used.
![]() Payer Address - In these fields - Street Address, City, State, and Zip Code - enter the payer's address.
Payer Address - In these fields - Street Address, City, State, and Zip Code - enter the payer's address.
![]() Receiver ID (Interchange Receiver ID - ISA08) - In this field, type the payer's receiver ID. This is an ID number belonging to the insurance company or payer, and can be retrieved from them.
Receiver ID (Interchange Receiver ID - ISA08) - In this field, type the payer's receiver ID. This is an ID number belonging to the insurance company or payer, and can be retrieved from them.
![]() Receiver Code (Application Receiver's Code - GS03) - In this field, type the payer's receiver code. If nothing is entered here the receiver ID will be used as the payer's receiver code as well as the receiver ID.
Receiver Code (Application Receiver's Code - GS03) - In this field, type the payer's receiver code. If nothing is entered here the receiver ID will be used as the payer's receiver code as well as the receiver ID.
![]() Receiver Identification Code (NM1*40-09) - In this field, type the receiver identification code. If nothing is entered the Receiver ID will be used as both the receiver ID and the payer's receiver identification code.
Receiver Identification Code (NM1*40-09) - In this field, type the receiver identification code. If nothing is entered the Receiver ID will be used as both the receiver ID and the payer's receiver identification code.
![]() Payer ID (Payers Identification Code - NM1*PR-09) - In this field enter the payer's ID number. If nothing is entered here, the Receiver ID will be used as the payer's ID as well as the receiver ID.
Payer ID (Payers Identification Code - NM1*PR-09) - In this field enter the payer's ID number. If nothing is entered here, the Receiver ID will be used as the payer's ID as well as the receiver ID.
![]() Claim Filing Indicator Code (SBR09) - In this field, type the code to submit in the 837 claim file. If nothing is entered here AWARDS will submit the code as follows:
Claim Filing Indicator Code (SBR09) - In this field, type the code to submit in the 837 claim file. If nothing is entered here AWARDS will submit the code as follows:
MB - If the payer is Medicare
MC - If the payer contains "Medicaid"
ZZ - If the payer starts with "Tenncare"
BL - If the payer contains "Blue" or "BC/BS"
CH - If the payer contains "Champus"
16 - If the payer contains "Healthfirst"
ZZ - For all other payer names
![]() Override Trading Partner ID Qualifier ZZ in 837 (ISA05) - In this field enter the two-character alphanumeric qualifier as requested by the payer. If left blank, "ZZ" will be inserted in the 837 claim file by default.
Override Trading Partner ID Qualifier ZZ in 837 (ISA05) - In this field enter the two-character alphanumeric qualifier as requested by the payer. If left blank, "ZZ" will be inserted in the 837 claim file by default.
![]() Override Interchange ID Qualifier ZZ in 837 (ISA07) - In this field enter the two-digit qualifier as requested by the payer. If left blank, "ZZ" will be inserted in the 837 claim file by default.
Override Interchange ID Qualifier ZZ in 837 (ISA07) - In this field enter the two-digit qualifier as requested by the payer. If left blank, "ZZ" will be inserted in the 837 claim file by default.
![]() Billing Provider Name (NM1*85) - If it is necessary to report a specific name in the 837 file, enter the agency name in this field. If left blank, the default (agency name associated with the database) will be used. The data from this field will also populate box 33 of the HCFA-1500 claim form.
Billing Provider Name (NM1*85) - If it is necessary to report a specific name in the 837 file, enter the agency name in this field. If left blank, the default (agency name associated with the database) will be used. The data from this field will also populate box 33 of the HCFA-1500 claim form.
![]() Report Service Facility Info in 837 (NMI*77) - Click this checkbox to send service facility information in the 837I and/or 837P electronic claim file. The service facility information data (address, city, state, zip code) is pulled from the System Setup > Agency Program Information > Address/Contact Information tab for a program. The service facility NPI data is pulled from the BillingBuilder > Program Billing Info > Service Facility NPI field.
Report Service Facility Info in 837 (NMI*77) - Click this checkbox to send service facility information in the 837I and/or 837P electronic claim file. The service facility information data (address, city, state, zip code) is pulled from the System Setup > Agency Program Information > Address/Contact Information tab for a program. The service facility NPI data is pulled from the BillingBuilder > Program Billing Info > Service Facility NPI field.
When this option is checked, the following additional options are made available on the page:
Service Facility Provider Name - If necessary, enter the name of the service facility provider in this text box. If left blank, the program name will be reported in the 837 file (as pulled from the Program Name field under System Setup > Agency Program Information > Add/Edit Entire Program > General Settings tab.)
Report Service Facility Secondary ID (REF) - Click this checkbox to report a service facility secondary ID in the 837 claim file for this payer (as pulled from procedure configuration > Service Facility Secondary ID setting - and/or - program billing info > Service Facility Secondary ID setting).
![]() Report Billing Provider Taxonomy Code in 837 (PRV*BI*PXC (837I and 837P)) - Click this checkbox to submit the billing provider's taxonomy code in the 837 claim file. This taxonomy code info is pulled from the "Taxonomy Code" field under Program Billing Groups configuration (for the program billing group associated with the generated batch of invoices).
Report Billing Provider Taxonomy Code in 837 (PRV*BI*PXC (837I and 837P)) - Click this checkbox to submit the billing provider's taxonomy code in the 837 claim file. This taxonomy code info is pulled from the "Taxonomy Code" field under Program Billing Groups configuration (for the program billing group associated with the generated batch of invoices).
![]() Report Rendering/Attending Taxonomy Code in 837 (PRV*AT*PXC*837I) / PRV*PE*PXC (837P)) - Click this checkbox to submit the rendering or attending provider's taxonomy code in the 837 claim file. The taxonomy code reported will be based on the Rendering/Attending NPI associated with the invoice; specifically, if the Rending/Attending NPI associated with the invoice is reported from one of the following locations, the taxonomy code from that same location will be included:
Report Rendering/Attending Taxonomy Code in 837 (PRV*AT*PXC*837I) / PRV*PE*PXC (837P)) - Click this checkbox to submit the rendering or attending provider's taxonomy code in the 837 claim file. The taxonomy code reported will be based on the Rendering/Attending NPI associated with the invoice; specifically, if the Rending/Attending NPI associated with the invoice is reported from one of the following locations, the taxonomy code from that same location will be included:
Human Resources > National Provider Identifier
BillingBuilder Procedures Setup > Incident to NPI
BillingBuilder Program Billing Info > Default Medical Provider Information
![]() Report Rendering/Attending Provider Secondary ID in 837 (REF) - Click this checkbox to report a secondary ID and ID qualifier within the 837P and 837I files for the rendering provider (837P) and attending provider (837I). This data is reported in the "REF" 837 segment within the 2310B loop (837P) and the 2310A loop (837I).
Report Rendering/Attending Provider Secondary ID in 837 (REF) - Click this checkbox to report a secondary ID and ID qualifier within the 837P and 837I files for the rendering provider (837P) and attending provider (837I). This data is reported in the "REF" 837 segment within the 2310B loop (837P) and the 2310A loop (837I).
![]() Report Hierarch Parent HL ID in HL02 of 837 for both Subscriber and Patient HL segments - Click this checkbox if subscriber data is being reported to this payer and the consumer is not always the subscriber. Typically used for commercial insurance plans.
Report Hierarch Parent HL ID in HL02 of 837 for both Subscriber and Patient HL segments - Click this checkbox if subscriber data is being reported to this payer and the consumer is not always the subscriber. Typically used for commercial insurance plans.
![]() Report Claim Frequency Type Code 7 on Denial Re-bill Invoices (CLM05-03) - Click this checkbox to send all invoices that have been marked as re-bill in a remittance worksheet as "Adjusted" invoices (CLM05-03 =7), and provide the payer's original CCN (claim control number) in the 837 claim file.
Report Claim Frequency Type Code 7 on Denial Re-bill Invoices (CLM05-03) - Click this checkbox to send all invoices that have been marked as re-bill in a remittance worksheet as "Adjusted" invoices (CLM05-03 =7), and provide the payer's original CCN (claim control number) in the 837 claim file.
![]() TIP: Only use this setting if requested by your payer, as invoice data will not reflect "new" invoices.
TIP: Only use this setting if requested by your payer, as invoice data will not reflect "new" invoices.
![]() Report "0" in Box 21 of HCFA-1500 - Click this checkbox to report 0 in box 21 of the HCFA-1500 paper claim form instead of the default of 10 for an ICD-10 diagnosis code.
Report "0" in Box 21 of HCFA-1500 - Click this checkbox to report 0 in box 21 of the HCFA-1500 paper claim form instead of the default of 10 for an ICD-10 diagnosis code.
![]() Report Rendering Provider Additional ID/Code in Box 24J (shaded area) of HCFA-1500 - Click the appropriate radio button to indicate what data needs to be reported in box 24j (the shaded area) of the HCFA-1500. Available options are:
Report Rendering Provider Additional ID/Code in Box 24J (shaded area) of HCFA-1500 - Click the appropriate radio button to indicate what data needs to be reported in box 24j (the shaded area) of the HCFA-1500. Available options are:
Leave Blank - When selected, no data is reported.
Rendering Provider Secondary ID - When selected, the rendering provider's secondary ID is reported. Depending on where the invoice rendering/attending NPI is reported from, the associated secondary ID will be included:
- Human Resources > Staff Information > Credentials > Rendering/Attending Provider Secondary ID
- Program Billing Info > Default Medical Providers Information > Secondary ID
- Edit Procedures > Incident to Secondary ID
Rendering Provider Taxonomy Code - When selected, the rendering provider's taxonomy code is reported. Depending on where the invoice rendering/attending NPI is reported from, the associated taxonomy will be included:
- Human Resources > Staff Information > Credentials > Taxonomy Code
- Program Billing Info > Default Medical Providers Information > Taxonomy Code
- Edit Procedures > Incident to Taxonomy Code
![]() Report Multiple Invoices on HCFA-1500 and UB-04 Per Consumer - Check this checkbox to report more than one invoice/procedure per HCFA-1500 or UB-04 paper claim form from a single invoice batch.
Report Multiple Invoices on HCFA-1500 and UB-04 Per Consumer - Check this checkbox to report more than one invoice/procedure per HCFA-1500 or UB-04 paper claim form from a single invoice batch.
![]() NOTE: The following restrictions may cause invoices/procedure codes for an individual client in a single invoice batch to be reported on more than one form:
NOTE: The following restrictions may cause invoices/procedure codes for an individual client in a single invoice batch to be reported on more than one form:
HCFA-1500
- Rendering provider data in box 31 is different (also NPI in box 24J is different)
- Service facility address in box 32 is different
- Invoices are a mixture of both ICD-9/ICD-10 codes in box 21
UB-04
- Attending provider data in box 76 is different
![]() Report Sender Address from Program Billing Groups in Box 2 of UB-04 - Click this checkbox to report the sender's address from the program billing groups in box 2 of the UB-04. Additionally, the sender's phone number from the billing type will be reported as well as the billing provider's name.
Report Sender Address from Program Billing Groups in Box 2 of UB-04 - Click this checkbox to report the sender's address from the program billing groups in box 2 of the UB-04. Additionally, the sender's phone number from the billing type will be reported as well as the billing provider's name.
![]() Report Consumers Name in Box 8a of UB-04 - Click this checkbox to report the consumer's name in box 8a of the UB-04 in place of the default data, the consumer's SSN.
Report Consumers Name in Box 8a of UB-04 - Click this checkbox to report the consumer's name in box 8a of the UB-04 in place of the default data, the consumer's SSN.
![]() Report Payer Name and Address Information in Box 38 of UB-04 - Click this checkbox to report the payer's name and the payer's address within box 38 of the UB-04 claim form.
Report Payer Name and Address Information in Box 38 of UB-04 - Click this checkbox to report the payer's name and the payer's address within box 38 of the UB-04 claim form.
![]() Report Locator Code from Program Billing Info in Box 51 of UB-04 - Click this checkbox to report the locator code from the Program Billing Info screen in box 51 of the UB-04 claim form.
Report Locator Code from Program Billing Info in Box 51 of UB-04 - Click this checkbox to report the locator code from the Program Billing Info screen in box 51 of the UB-04 claim form.
![]() Show Additional Configuration Options on Configure Billing Types Screen - Click this checkbox to enable additional 837I file options to be shown when Configuring Billing Types.
Show Additional Configuration Options on Configure Billing Types Screen - Click this checkbox to enable additional 837I file options to be shown when Configuring Billing Types.
![]() Entitlements Eligibility ID Entry Format - Click this drop-down arrow and make a selection to indicate whether the entitlements identifier format should be "numbers," "letters," or "numbers and letters."
Entitlements Eligibility ID Entry Format - Click this drop-down arrow and make a selection to indicate whether the entitlements identifier format should be "numbers," "letters," or "numbers and letters."
![]() TIP: The entitlements identifier format set here will determine which format can be used when entering ID numbers using the Entitlements module Certified Entitlements feature. For example, if "numbers" is selected and users enter letters in an entitlement's ID field, they will receive an error and the information will not be saved.
TIP: The entitlements identifier format set here will determine which format can be used when entering ID numbers using the Entitlements module Certified Entitlements feature. For example, if "numbers" is selected and users enter letters in an entitlement's ID field, they will receive an error and the information will not be saved.
![]() Payer Contact Information (not used in claims) - In this field, type the payer's contact information.
Payer Contact Information (not used in claims) - In this field, type the payer's contact information.
The process of configuring payers is now complete.
![]() TIP: If it is later necessary to update or delete a payer, complete steps 1 through 3 above, select the appropriate payer from the Payer selection list, and then click UPDATE or DELETE, respectively. Keep in mind:
TIP: If it is later necessary to update or delete a payer, complete steps 1 through 3 above, select the appropriate payer from the Payer selection list, and then click UPDATE or DELETE, respectively. Keep in mind:
![]() When updating - The payer name cannot be changed but all other payer detail can be updated as needed. If any changes are made, you must be sure to click SAVE to have those changes applied.
When updating - The payer name cannot be changed but all other payer detail can be updated as needed. If any changes are made, you must be sure to click SAVE to have those changes applied.
![]() When deleting - A payer can only be deleted if there are no billing types, procedures, rates, or programs associated with it. If you choose to delete a payer with which none of those items are associated, you will be shown a confirmation page after clicking DELETE. Be sure to click OK on that page to complete the deletion process. Once deleted, a payer cannot be restored.
When deleting - A payer can only be deleted if there are no billing types, procedures, rates, or programs associated with it. If you choose to delete a payer with which none of those items are associated, you will be shown a confirmation page after clicking DELETE. Be sure to click OK on that page to complete the deletion process. Once deleted, a payer cannot be restored.
https://demodb.footholdtechnology.com/help/?11425