|   |
|   |
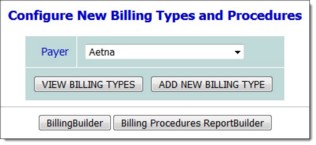
Once payers have been added to the system, billing types must be configured for each of them. In general, billing types correspond to different types of services. Keep in mind while completing this step that in some cases a single payer will need to have multiple billing types set up for it. (For example, Medicaid pays for clinic services and day treatment services, each of which would need to be configured as a separate billing type for Medicaid.) Also note that while multiple payers may have the same billing type, that type must be set up separately for each.
To configure a new billing type, complete the following steps:
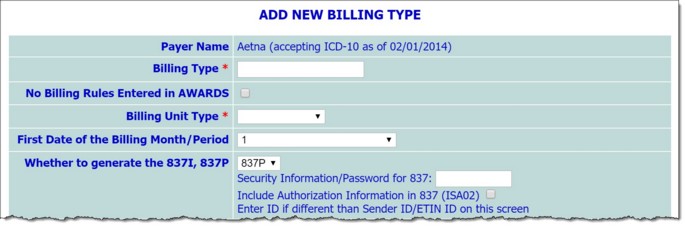
![]() IMPORTANT! In order to complete a claim successfully, the Whether to generate the 837I, 837P, Sender ID/ETIN, Agency Tax ID, and Sender Location Code fields must be completed, in addition to the fields required by AWARDS.
IMPORTANT! In order to complete a claim successfully, the Whether to generate the 837I, 837P, Sender ID/ETIN, Agency Tax ID, and Sender Location Code fields must be completed, in addition to the fields required by AWARDS.
![]() Billing Type - In this field, type the name of the billing type; for example, "Outpatient Clinic." Be sure to enter the name carefully, as once saved it cannot be changed.
Billing Type - In this field, type the name of the billing type; for example, "Outpatient Clinic." Be sure to enter the name carefully, as once saved it cannot be changed.
![]() No Billing Rules Entered in AWARDS - Click this checkbox if this billing type will have no procedures or documentation requirements entered in AWARDS.
No Billing Rules Entered in AWARDS - Click this checkbox if this billing type will have no procedures or documentation requirements entered in AWARDS.
![]() TIP: The billing unit type does not refer to the frequency with which you will bill for services. It defines whether an invoice for a configured procedure will be generated daily (Daily/Per Diem) or once per month (Monthly). For example, if a procedure is configured for a billing type that has "Daily/Per Diem" selected as the billing unit type, the procedure can be billed once per day/consumer as a single-line invoice or as part of a multi-line invoice. If a procedure is configured for a billing type that has "Monthly" selected as the billing unit type, the procedure can be billed once per month/consumer as a single-line invoice or as part of a multi-line invoice.
TIP: The billing unit type does not refer to the frequency with which you will bill for services. It defines whether an invoice for a configured procedure will be generated daily (Daily/Per Diem) or once per month (Monthly). For example, if a procedure is configured for a billing type that has "Daily/Per Diem" selected as the billing unit type, the procedure can be billed once per day/consumer as a single-line invoice or as part of a multi-line invoice. If a procedure is configured for a billing type that has "Monthly" selected as the billing unit type, the procedure can be billed once per month/consumer as a single-line invoice or as part of a multi-line invoice.
![]() First Date of the Billing Month/Period - Select the start date for monthly billing. The default value is "1" for the first of the month.
First Date of the Billing Month/Period - Select the start date for monthly billing. The default value is "1" for the first of the month.
![]() NOTE: This option is only available when "Monthly" has been selected from the Billing Unit Type drop-down on this page.
NOTE: This option is only available when "Monthly" has been selected from the Billing Unit Type drop-down on this page.
![]() Monthly billing primary invoices invoice date - Click this drop-down arrow and make a selection to indicate whether primary invoices should be dated with "The first day of the next month/billing period," "The first day of the current month/billing period," "The last day of the current month/billing period," and "The date on which the service was first provided in the current month/billing period."
Monthly billing primary invoices invoice date - Click this drop-down arrow and make a selection to indicate whether primary invoices should be dated with "The first day of the next month/billing period," "The first day of the current month/billing period," "The last day of the current month/billing period," and "The date on which the service was first provided in the current month/billing period."
![]() NOTE: This option is only available when "Monthly" has been selected from the Billing Unit Type drop-down on this page.
NOTE: This option is only available when "Monthly" has been selected from the Billing Unit Type drop-down on this page.
![]() Monthly billing add on invoices invoice date - Click this drop-down arrow and make a selection to indicate whether additional invoices should be dated with "The invoice date of the primary invoice," or "The date of service."
Monthly billing add on invoices invoice date - Click this drop-down arrow and make a selection to indicate whether additional invoices should be dated with "The invoice date of the primary invoice," or "The date of service."
![]() NOTE: This option is only available when "Monthly" has been selected from the Billing Unit Type drop-down on this page.
NOTE: This option is only available when "Monthly" has been selected from the Billing Unit Type drop-down on this page.
![]() TIP: The 837I and 837P formats are standard national file formats for billing claims. Most AWARDS agencies will use the 837I format, since the 837P is the format for services provided and billed by professionals, such as a doctor's office.
TIP: The 837I and 837P formats are standard national file formats for billing claims. Most AWARDS agencies will use the 837I format, since the 837P is the format for services provided and billed by professionals, such as a doctor's office.
![]() Security Information/Password for 837 - Some billing types require a password in order to submit claim files. If needed, enter the password in this field, which will accept up to ten characters.
Security Information/Password for 837 - Some billing types require a password in order to submit claim files. If needed, enter the password in this field, which will accept up to ten characters.
![]() Include Authorization Information in 837 (ISA02) - Click this checkbox to include the Sender ID/ETIN/Submitter ID in the 837 claim file.
Include Authorization Information in 837 (ISA02) - Click this checkbox to include the Sender ID/ETIN/Submitter ID in the 837 claim file.
![]() Enter ID if different than Sender ID/ETIN on this screen - Enter the ID needed in ISA02 of the 837 file if the ID is not the same as the Sender ID/ETIN on this screen.
Enter ID if different than Sender ID/ETIN on this screen - Enter the ID needed in ISA02 of the 837 file if the ID is not the same as the Sender ID/ETIN on this screen.
![]() Which Axis to Include - Select the diagnosis type to be used for billing invoices. Available options are:
Which Axis to Include - Select the diagnosis type to be used for billing invoices. Available options are:
Axis I (not after 10/1/2015) - Click this radio button to use DSM-IV - Axis I for billing invoices.
Axis II (not after 10/1/2015) - Click this radio button to use DSM-IV - Axis II for billing invoices.
No DSM-IV Axis (on or before 10/1/2015) - Click this radio button to NOT use DSM-IV for billing invoices.
DSM 5 (on or before 10/1/2015) - Click this checkbox to use DSM 5 for billing invoices.
The first three options are radio buttons, so only one can be selected. The DSM 5 checkbox can be used in tandem with one of those first three options. This allows AWARDS to use either DSM 5 or DSM-IV diagnosis codes for billing invoices.
![]() Valid Diagnoses DSM/ICD Heading - In this field, type a comma delimited list of the ICD diagnoses required for this billing type. For example, if you are allowed to bill ICD codes that begin with F, S, and Q, then enter F,S,Q here. If you are allowed to bill only ICD codes that begin with F3, enter F3 here.
Valid Diagnoses DSM/ICD Heading - In this field, type a comma delimited list of the ICD diagnoses required for this billing type. For example, if you are allowed to bill ICD codes that begin with F, S, and Q, then enter F,S,Q here. If you are allowed to bill only ICD codes that begin with F3, enter F3 here.
![]() Sender ID/ETIN - In this field, type the sender ID/ETIN (or Electronic Transmitter Identification Number). This ID belongs to the agency, and identifies the agency to the payers.
Sender ID/ETIN - In this field, type the sender ID/ETIN (or Electronic Transmitter Identification Number). This ID belongs to the agency, and identifies the agency to the payers.
![]() Provider ID - In this field, type the provider's ID number.
Provider ID - In this field, type the provider's ID number.
![]() Sender Address - In this field, type the sender's address using the following format: Street Address, City, State Abbreviation Zip Code. (For example, a correctly formatted address would read: 123 Main Street, New York, NY 100036020.)
Sender Address - In this field, type the sender's address using the following format: Street Address, City, State Abbreviation Zip Code. (For example, a correctly formatted address would read: 123 Main Street, New York, NY 100036020.)
![]() Sender's Phone Number - In this field, type the sender's phone number.
Sender's Phone Number - In this field, type the sender's phone number.
![]() Sender location code - In this field, type the sender's location code.
Sender location code - In this field, type the sender's location code.
![]() NOTE: The location code is a legacy value used by NY State Medicaid in the MMIS system, which has been replaced in the claim files by the CMS place of service code, except for PWDD - MSC claims. This field only applies to programs doing PWDD - MSC billing in the state of NY.
NOTE: The location code is a legacy value used by NY State Medicaid in the MMIS system, which has been replaced in the claim files by the CMS place of service code, except for PWDD - MSC claims. This field only applies to programs doing PWDD - MSC billing in the state of NY.
![]() CMS place of service code (837P)/Uniform Bill Type Code (837I) - For 837P billing types enter the CMS place of service code in this field. For 837I billing types, enter the NUBC code. If the payer for this billing type is self-pay, enter "0" in this field.
CMS place of service code (837P)/Uniform Bill Type Code (837I) - For 837P billing types enter the CMS place of service code in this field. For 837I billing types, enter the NUBC code. If the payer for this billing type is self-pay, enter "0" in this field.
![]() TIP: The CMS place of service code is a code that defines the type of facility where the service is being provided. For more information, including a table of these codes, please refer to the following website: http://www.cms.hhs.gov/PlaceofServiceCodes/
TIP: The CMS place of service code is a code that defines the type of facility where the service is being provided. For more information, including a table of these codes, please refer to the following website: http://www.cms.hhs.gov/PlaceofServiceCodes/
![]() Report Telehealth Modifier Code in 837 Claim File - In this field, enter the two-character Telehealth modifier code that needs to be included in the 837 claim file for this billing types procedures.
Report Telehealth Modifier Code in 837 Claim File - In this field, enter the two-character Telehealth modifier code that needs to be included in the 837 claim file for this billing types procedures.
![]() NOTE: This setting is only available when "No Billing Rules Entered in AWARDS" is selected on this same page. Also, this setting only applies to hard coded ACT, CR, and PROS billing to NYS Medicaid and MCO Medicaid payers.
NOTE: This setting is only available when "No Billing Rules Entered in AWARDS" is selected on this same page. Also, this setting only applies to hard coded ACT, CR, and PROS billing to NYS Medicaid and MCO Medicaid payers.
![]() NOTE: The Telehealth modifier code entered in this field will be reported in the c837 claim file for a consumer's invoice if at least one for the notes used to generate the invoice includes "Telehealth" as a Location (PROS and CR), or "Telehealth" as a Contact Method (ACT).
NOTE: The Telehealth modifier code entered in this field will be reported in the c837 claim file for a consumer's invoice if at least one for the notes used to generate the invoice includes "Telehealth" as a Location (PROS and CR), or "Telehealth" as a Contact Method (ACT).
![]() 837I/UB-04 Value Code - Enter a valid code here to be reported in both the 837I and the UB-04 claim formats. The default code reported is "24." This code will be inserted in the following locations in the claim files/forms:
837I/UB-04 Value Code - Enter a valid code here to be reported in both the 837I and the UB-04 claim formats. The default code reported is "24." This code will be inserted in the following locations in the claim files/forms:
837 file - HI*BE segment
UB-04 - Box 39/40/41- code column
![]() Send Invoice Amount in Box 39(amount)/40(amount)/41(amount) of UB-04 - Click this checkbox to report the sum of all invoice/procedure amounts in the UB-04. The default information comes from the Rate/Procedure Code associated with the invoice and the first four characters of that code.
Send Invoice Amount in Box 39(amount)/40(amount)/41(amount) of UB-04 - Click this checkbox to report the sum of all invoice/procedure amounts in the UB-04. The default information comes from the Rate/Procedure Code associated with the invoice and the first four characters of that code.
![]() Send Spend Down Amount in HI*BE 01-05 of 837I - Click this checkbox to report the consumer's spend down amount in the HI segment of the 837I claim file. The data for this segment comes from the consumer's Certified Entitlement record > Miscellaneous Entitlements / Eligibilities / Subsidies section. An eligibility called "Spend Down" needs to be assigned to the consumer with an amount entered and an effective date that is on or before the date of service being billed. Please contact the AWARDS help desk to have the "Spend Down" misc. entitlement added to your database if needed.
Send Spend Down Amount in HI*BE 01-05 of 837I - Click this checkbox to report the consumer's spend down amount in the HI segment of the 837I claim file. The data for this segment comes from the consumer's Certified Entitlement record > Miscellaneous Entitlements / Eligibilities / Subsidies section. An eligibility called "Spend Down" needs to be assigned to the consumer with an amount entered and an effective date that is on or before the date of service being billed. Please contact the AWARDS help desk to have the "Spend Down" misc. entitlement added to your database if needed.
![]() Send Admitting Diagnosis in 837I and UB-04 - Click this checkbox to submit diagnosis information in the 837I (HI*ABJ segment) and the UB-04 (box 69).
Send Admitting Diagnosis in 837I and UB-04 - Click this checkbox to submit diagnosis information in the 837I (HI*ABJ segment) and the UB-04 (box 69).
![]() NOTE:This option is only available when Whether to generate the 837I, 837P is set to "837I."
NOTE:This option is only available when Whether to generate the 837I, 837P is set to "837I."
![]() Send Admission Date in 837I and UB-04 - Click this checkbox to send the consumer's admission date (to the program associated with the invoice billing billed) in both the electronic 837I file and UB-04 paper claim form. Also select the Include Admission Hour checkbox to report an admission hour alongside the admission date.
Send Admission Date in 837I and UB-04 - Click this checkbox to send the consumer's admission date (to the program associated with the invoice billing billed) in both the electronic 837I file and UB-04 paper claim form. Also select the Include Admission Hour checkbox to report an admission hour alongside the admission date.
![]() NOTE:These options are only available when Whether to generate the 837I, 837P is set to "837I."
NOTE:These options are only available when Whether to generate the 837I, 837P is set to "837I."
![]() Send Discharge Hour in 837I (DTP*096) - Click this checkbox to include the discharge hour information and segment (DTP*096) in the 837I claim file.
Send Discharge Hour in 837I (DTP*096) - Click this checkbox to include the discharge hour information and segment (DTP*096) in the 837I claim file.
![]() For Discharged clients use Discharge Date - Only available for ACT programs. If this option is checked, invoices for discharged clients will be dated on the date of discharge.
For Discharged clients use Discharge Date - Only available for ACT programs. If this option is checked, invoices for discharged clients will be dated on the date of discharge.
![]() All programs with this billing type use the same billing rates - Click this checkbox if multiple programs will be assigned to the same program billing group that uses this payer's billing type, and the billing rates are the same for all programs. This setting allows billing rates to be entered for one program assigned to the payer's program billing and to have the billing rates apply to all programs within the program billing group.
All programs with this billing type use the same billing rates - Click this checkbox if multiple programs will be assigned to the same program billing group that uses this payer's billing type, and the billing rates are the same for all programs. This setting allows billing rates to be entered for one program assigned to the payer's program billing and to have the billing rates apply to all programs within the program billing group.
![]() Prior Authorization Required? - Only available for hard-coded ACT and PROS billing types where the payer name includes "Medicaid." If hard-coded ACT or PROS procedures are selected, an authorization record needs to exist within the consumer's entitlements in order for the procedure(s) to be invoiced. This setting is used to add an additional billing requirement to generate invoices as well as report the authorization number from the consumer's authorization record in the 837I and UB-04.
Prior Authorization Required? - Only available for hard-coded ACT and PROS billing types where the payer name includes "Medicaid." If hard-coded ACT or PROS procedures are selected, an authorization record needs to exist within the consumer's entitlements in order for the procedure(s) to be invoiced. This setting is used to add an additional billing requirement to generate invoices as well as report the authorization number from the consumer's authorization record in the 837I and UB-04.
![]() TIP: The referring provider for each client is entered using the Support Services Contacts section of his or her face sheet.
TIP: The referring provider for each client is entered using the Support Services Contacts section of his or her face sheet.
![]() Default Referring Provider ID - In this field, type the provider ID that should be used if no provider ID or license number is found for the Authorizing Psychiatrist/Nurse/Provider for the client in the Supportive Services Contacts information (located on the client's face sheet).
Default Referring Provider ID - In this field, type the provider ID that should be used if no provider ID or license number is found for the Authorizing Psychiatrist/Nurse/Provider for the client in the Supportive Services Contacts information (located on the client's face sheet).
![]() NOTE: This field is only available when the Referring provider is required option has been checked off.
NOTE: This field is only available when the Referring provider is required option has been checked off.
![]() Allow multiline invoices for add on procedures? - Click this drop-down arrow and select "Yes" or "No" to indicate whether multi-line invoices should be allowed for this billing type. If this field is set to "Yes," enter a number value in the If yes, indicate the limit of multiple lines field to indicate any limit on how many lines should be allowed. If no value is entered in this field, there will be no limit put in place. If applicable, click the Create after hours modifier line using CPT/HCPCS checkbox and enter the related code in the corresponding field to the right of the option label.
Allow multiline invoices for add on procedures? - Click this drop-down arrow and select "Yes" or "No" to indicate whether multi-line invoices should be allowed for this billing type. If this field is set to "Yes," enter a number value in the If yes, indicate the limit of multiple lines field to indicate any limit on how many lines should be allowed. If no value is entered in this field, there will be no limit put in place. If applicable, click the Create after hours modifier line using CPT/HCPCS checkbox and enter the related code in the corresponding field to the right of the option label.
![]() NOTE: These fields are only available when the Billing Unit Type has been set to either "Monthly" or "Daily/Per Diem." These fields apply to New York state clinic billing. If your agency does not need to use these options, leave them blank or set to "No."
NOTE: These fields are only available when the Billing Unit Type has been set to either "Monthly" or "Daily/Per Diem." These fields apply to New York state clinic billing. If your agency does not need to use these options, leave them blank or set to "No."
![]() Use Cascading Insurance Authorizations - Click this checkbox to enable the Cascading Authorizations feature in authorizations data entry. When checked, users will have the option to activate the cascading authorizations feature using a "Cascading Auth?" option in the BillingBuilder Insurance Authorizations portion of a consumer's Certified Entitlements. This option allows a single authorization record for a consumer to have distinct authorization periods with distinct authorized units. When using this option, unbilled units from past periods are allowed to be billed/invoiced in newer and current periods.
Use Cascading Insurance Authorizations - Click this checkbox to enable the Cascading Authorizations feature in authorizations data entry. When checked, users will have the option to activate the cascading authorizations feature using a "Cascading Auth?" option in the BillingBuilder Insurance Authorizations portion of a consumer's Certified Entitlements. This option allows a single authorization record for a consumer to have distinct authorization periods with distinct authorized units. When using this option, unbilled units from past periods are allowed to be billed/invoiced in newer and current periods.
![]() No COB: Treat Payer as Primary - Click this checkbox if this billing type does not allow COB (coordination of benefits) billing. All invoices associated with this billing type will be using the payer associated with this billing type as primary in the claim file (even if the payer is set as Secondary or Tertiary within the Entitlements records for the client). Future batches are not allowed for this billing type/payer.
No COB: Treat Payer as Primary - Click this checkbox if this billing type does not allow COB (coordination of benefits) billing. All invoices associated with this billing type will be using the payer associated with this billing type as primary in the claim file (even if the payer is set as Secondary or Tertiary within the Entitlements records for the client). Future batches are not allowed for this billing type/payer.
![]() Additional Value Code Digits - Click this checkbox to submit extra digits with the value code sent in the 837I (HI*BE:24) claim file. Please note, this option is only available if "Show Additional Configuration Options on Configure Billing Types Screen" has been checked under Configure Payers.
Additional Value Code Digits - Click this checkbox to submit extra digits with the value code sent in the 837I (HI*BE:24) claim file. Please note, this option is only available if "Show Additional Configuration Options on Configure Billing Types Screen" has been checked under Configure Payers.
![]() Omit Patient's Reason for Visit Diagnosis in 837I - Click this checkbox to omit this data in the 837I claim file. When checked the HI*APR segment of the 837I will not be included. Please note, this option is only available if "Show Additional Configuration Options on Configure Billing Types Screen" has been checked under Configure Payers for the payer associated with this billing type.
Omit Patient's Reason for Visit Diagnosis in 837I - Click this checkbox to omit this data in the 837I claim file. When checked the HI*APR segment of the 837I will not be included. Please note, this option is only available if "Show Additional Configuration Options on Configure Billing Types Screen" has been checked under Configure Payers for the payer associated with this billing type.
![]() Omit Rate/Procedure Code from Box 44 of UB-04 - Click this checkbox to omit the Rate/Procedure Code data from box 44 of the UB-04 claim form. The data entered within the Rate/Procedure Code field of the procedure being invoiced is reported by default.
Omit Rate/Procedure Code from Box 44 of UB-04 - Click this checkbox to omit the Rate/Procedure Code data from box 44 of the UB-04 claim form. The data entered within the Rate/Procedure Code field of the procedure being invoiced is reported by default.
![]() Omit ICD-10 DX Code in Box 67A of UB-04 - Click this checkbox to omit the invoice ICD-10 code from box 67A of the UB-04 claim form. The invoice ICD-10 code is reported by default.
Omit ICD-10 DX Code in Box 67A of UB-04 - Click this checkbox to omit the invoice ICD-10 code from box 67A of the UB-04 claim form. The invoice ICD-10 code is reported by default.
![]() Override CL103 in 837I - Enter a code in this field that will be reported in place of the default code of "30" in the CL1 segment of the 837I claim file. If a value is not entered, AWARDS will report the default code of "30." Please note, this option is only available if "Show Additional Configuration Options on Configure Billing Types Screen" has been checked under Configure Payers for the payer associated with this billing type.
Override CL103 in 837I - Enter a code in this field that will be reported in place of the default code of "30" in the CL1 segment of the 837I claim file. If a value is not entered, AWARDS will report the default code of "30." Please note, this option is only available if "Show Additional Configuration Options on Configure Billing Types Screen" has been checked under Configure Payers for the payer associated with this billing type.
![]() Create Split Invoices for All Responsible Parties - Click this checkbox to create split self-pay invoices when the consumer has the additional "Self-Pay" eligibilities entered in their entitlements. These additional eligibilities need to be added by the AWARDS Help Desk and need to be labeled with the prefix "Self-Pay:" but can contain any additional responsible party label at the end.
Create Split Invoices for All Responsible Parties - Click this checkbox to create split self-pay invoices when the consumer has the additional "Self-Pay" eligibilities entered in their entitlements. These additional eligibilities need to be added by the AWARDS Help Desk and need to be labeled with the prefix "Self-Pay:" but can contain any additional responsible party label at the end.
For example, if your agency has multiple consumers where the mother and father are responsible for a portion of the consumer's invoices, your additional self-pay eligibilities could be "Self-Pay:Father" and "Self-Pay:Mother." When assigning these additional self-pay eligibilities to consumers, please be sure to do the following:
a) Enter the percentage to be billed to the responsible party using the Use Sliding Percent (%) field.
b) Set Is Consumer Responsible Party to "no." Once set to no, ensure all needed info is filled in correctly for the responsible party information fields. That information will be used in place of the consumer's information on the consumer summary/statement for mailing purposes.
![]() TIP: The confirmation page includes a CONTINUE AND ADD PROCEDURES button, allowing you to begin part 4 in the BillingBuilder setup process directly from there. If you choose to add the procedures for this billing type at this time (rather than adding all billing types and then all procedures separately), click that button and proceed to number 8 under Configuring Procedures.
TIP: The confirmation page includes a CONTINUE AND ADD PROCEDURES button, allowing you to begin part 4 in the BillingBuilder setup process directly from there. If you choose to add the procedures for this billing type at this time (rather than adding all billing types and then all procedures separately), click that button and proceed to number 8 under Configuring Procedures.
![]() IMPORTANT! Even though multiple payers may have the same billing type, that billing type must be set up separately for each of them.
IMPORTANT! Even though multiple payers may have the same billing type, that billing type must be set up separately for each of them.
The process of configuring a new billing type is now complete.
![]() TIP: If it is later necessary to update or delete a billing type, complete steps 1 through 4 above, and then click VIEW BILLING TYPES. On the page that follows, select the billing type and click EDIT BILLING TYPE or DELETE BILLING TYPE as appropriate. Keep in mind:
TIP: If it is later necessary to update or delete a billing type, complete steps 1 through 4 above, and then click VIEW BILLING TYPES. On the page that follows, select the billing type and click EDIT BILLING TYPE or DELETE BILLING TYPE as appropriate. Keep in mind:
![]() When updating - The billing type name cannot be changed but all other billing type detail can be updated as needed. If any changes are made, you must be sure to click SAVE BILLING TYPE to have those changes applied.
When updating - The billing type name cannot be changed but all other billing type detail can be updated as needed. If any changes are made, you must be sure to click SAVE BILLING TYPE to have those changes applied.
![]() When deleting - A billing type can only be deleted if there are no procedures or program billing groups associated with it. If you choose to delete a billing type with which none of those items are associated, the deletion will occur as soon as DELETE BILLING TYPE is clicked. There is no confirmation page, and once deleted a billing type cannot be restored.
When deleting - A billing type can only be deleted if there are no procedures or program billing groups associated with it. If you choose to delete a billing type with which none of those items are associated, the deletion will occur as soon as DELETE BILLING TYPE is clicked. There is no confirmation page, and once deleted a billing type cannot be restored.
Want to view a report of billing procedure configurations, including any you just set up? See Using the Billing Procedures ReportBuilder.
https://demodb.footholdtechnology.com/help/?11426